Ayushman Bharat Yojana or the Pradhan Mantri Jan Arogya Yojana 2021 has been launched by the central government. The National Health Protection Scheme aims to provide health insurance coverage of up to Rs. 5 Lakh per year to vulnerable families. The central government under the Ayushman Bharat Yojana will cover around 100 million (10 Crore) poor and BPL families (Approximately 50 Crore Citizens) from across the country.
PM Jan Arogya Yojana or Ayushman Bharat Programme will provide cashless and paperless treatment for secondary and tertiary care hospitalization. The complete cost of the scheme implementation including the insurance premium will be borne by the central and state governments. Ayushman Bharat Treatment Package Rates are finalized by the central govt. and uploaded on the new NHPM Portal.
Along with providing cashless insurance benefits, the other component under the Ayushman Bharat Yojana includes opening of 1.5 Lakh health and wellness centers across the country to bring health services closer to people. These health and wellness centers will provide basic diagnostic services and essential drugs for free.
Ayushman Bharat Yojana Enrollment / Application / Registration
There is no need for any kind of enrollment, application or registration for availing the benefits of Ayushman Bharat Yojana. It is an eligibility based scheme under which the beneficiaries will be selected on the basis of different criteria including the SECC-2011 data. The eligibility for Ayushman Bharat Yojana can be checked by calling the helpline number at 14555 or by visiting the official “Am I Eligible” portal at mera.pmjay.gov.in.
Till date, there is yet no official notification regarding the online registration / applications for Ayushman Bharat Yojana. However, all those beneficiaries whose name appears in the PM Jan Arogya Yojana List can apply for Golden Cards. Now Ayushman Bharat Yojana Beneficiaries can also avail PMJAY services through Common Service Centers (CSCs).
How to Apply Online for Ayushman Bharat Yojana
There is no need to apply online or offline for Ayushman Bharat Yojana, it is an eligibility based scheme. There are no online application forms or registration being made for the scheme.
Ayushman Bharat Yojana Beneficiary Selection
The eligibility criteria of Ayushman Bharat Yojana is solely based on the Socio-Economic Caste Census (SECC) data covering both rural and urban areas across the country. The total number of the beneficiary families would be about 10.74 Crore consisting of deprived rural families and identified occupational category of urban workers’ families.
However, if the criteria of exclusion / inclusion / deprivation / occupation in SECC data is changed in future, the scheme will take into account all the changes and the beneficiary families will be included / excluded on the basis of same changed criteria. Also see the https://pmjay.gov.in/sites/default/files/2018-07/GuidelinesonProcessofBeneficiaryIdentification_0.pdf
Ayushman Bharat Yojana Coverage / Implementation
The National Health Protection Scheme / Mission under the Ayushman Bharat scheme will be implemented in all the states and union territories to cover all the targeted beneficiary families across the country. The programme will be implemented by the Ayushman Bharat National Health Protection Mission Agency (AB-NHPMA) under the supervision of Ministry of Health and Family Welfare, Government of India.
State Health Agency (SHA), newly formed or formed using an existing trust / society / no-profit company / state nodal agency would be responsible for the implementation of the scheme in respective state & UT’s. The cashless benefits of treatment under the scheme would be available in all the government hospitals and empaneled private hospitals except the negative list across the country.
Salient Features of Ayushman Bharat Yojana
Below are some of the main / salient features of Ayushman Bharat Yojana:-
- National Health Protection Mission and Health & Wellness Centers are the two major initiatives started under the Ayushman Bharat Scheme.
- National Health Protection Mission will provide insurance coverage of up to Rs. 5 Lakh per family per year for secondary and tertiary care hospitalization.
- 1.5 Lakh health and wellness centers would be started in health centers / hospitals across the country. More than 18 thousands already in operation.
- Over 10 Crore deprived rural and urban families (About 40% of the total population of the country) to be covered under the health insurance coverage scheme.
- The selection of beneficiaries to be done on the basis of SECC data.
- There will be no restriction on the size of the covered beneficiary family.
- The scheme will lead to timely treatment of the patient and increase in overall patient satisfaction. Overall efficiency and productivity of health care services will be improved thus improving the quality of life.
- The premium of the insurance coverage will be completely borne by the central and state governments based on the ration defined by the Ministry of Finance.
- State Health Agency (SHA) would be the responsible body for the implementation of the scheme in states.
- The cost of the treatments would be defined by the government in the advance as packages to control the cost.
- The benefits of the scheme would be portable across the country, meaning, a beneficiary can avail the cashless treatment at any government or empaneled private hospital in the country.
- To enable the paperless & cashless transaction, central government would establish a robust, modular, scalable and interoperable IT platform in partnership with NITI Aayog.
- Ayushman Bharat – National Health Protection Mission will subsume the on-going centrally sponsored schemes – Rashtriya Swasthya Bima Yojana (RSBY) and the Senior Citizen Health Insurance Scheme (SCHIS).
Check the complete Ayushman Bharat Yojana (PMJAY) Claim Settlement Guidelines in the section later.
Quick Facts & Information about Ayushman Bharat
| Data Point | Fact / Information |
|---|---|
| Name of Scheme / Initiative | Ayushman Bharat Scheme |
| Announced | 1 February 2018 by Prime Minister Narendra Modi |
| Launched | 23 September 2018 |
| Initiatives Under the Scheme | 1. National Health Protection Mission 2. Health & Wellness Centers |
| Implementing Authority | Ayushman Bharat National Health Protection Mission Agency (AB-NHPMA) under Ministry of Health and Family Welfare, Government of India |
| Scheme Coverage | All states and Union Territories |
| Budget Allocation | Rs. 6400 Crore in 2021-22 Union Budget |
| No. of Beneficiaries in NHPM | More than 10 Crore Families Under National Health Protection Mission Initiative |
| Benefits of NHPM | Health insurance coverage of up to Rs. 5 Lakh per annum per family for secondary & tertiary care hospitalization |
| Selection of Beneficiaries in NHPM | Deprived rural & identified occupational category of urban workers’ families as per SECC-2011 data |
| Size of covered beneficiary family in NHPM | No restriction on family size |
| Insurance premium for NHPM | Entire cost of premium to be borne by central & state governments |
| Treatment availability in NHPM | At all government & empaneled private hospitals |
| What is Health & Wellness Center | Health & wellness centers to provide basic health services / diagnostics & basic drugs for free. |
| Facilities at HWCs | Point of care for diagnostics / hub & spoke, wellness rooms for Yoga, Physiotherapy & group meetings, separate consulting space, free drug dispensation, telemedicine facilities, storage space for drugs & consumables and waiting area for 30+ people |
| No. of Health & Wellness centers | 1.5 Lakh total number to be started till December 2022 |
| Beneficiaries | All citizens of the country |
| More details | Ayushman Bharat Health & Wellness Centers |
More details about the Ayushman Bharat – National Health Protection Mission such as list of hospitals, list of beneficiaries is available on the official website at pmjay.gov.in.
About Pradhan Mantri Jan Arogya Yojana (PMJAY)
Prime Minister Narendra Modi launched Pradhan Mantri Jan Arogya Yojana (PMJAY) on 23 September 2018. This PMJAY Scheme is a mega National Health Protection Scheme (NHPS) for poor people. PMJAY will provide Rs. 5 Lakh health insurance for secondary and tertiary hospitalization. This Ayushman Bharat Yojana will benefit around 50 crore poor people and provide them cashless and paperless treatment in hospitals.
All the insured people can make claims for treatment in all empanelled hospitals and avail treatment at NHPM Treatment Package Rates. Pradhan Mantri Jan Arogya Yojana is applicable for all Rural and Urban Beneficaries whose name appears in SECC-2011 Data. There will be No Ayushman Bharat Yojana Online Application Forms and anti fraud guidelines are also framed against people who demand money to provide insurance benefits.
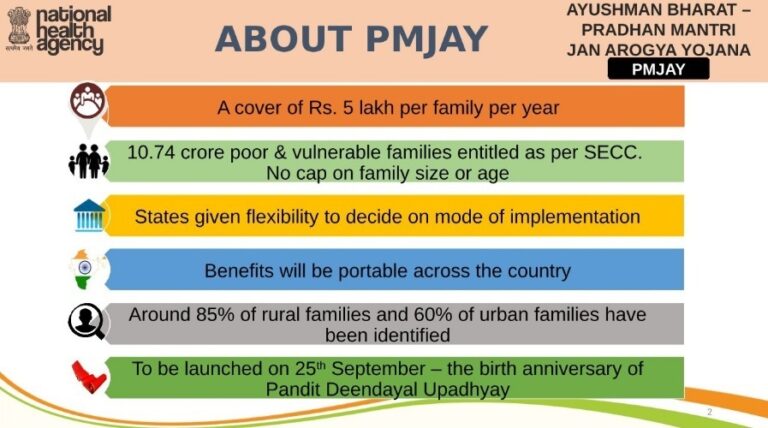
People can visit any Health and Wellness Center to avail PMJAY benefits. All the AB-NHPM beneficiaries will be given Ayushman Family Cards and Arogya Mitras will be trained for assistance. Check complete details regarding PMJAY Scheme here. The important features and highlights of Pradhan Mantri Jan Arogya Yojana are as follows:-
- Health Insurance cover of Rs. 5 lakh per family per year.
- Around 10.74 crore poor and vulnerable families whose name appears in the SECC-2011 Data are eligible. There is no cap on family size and age.
- States are given the flexibility to decide the mode of implementation.
- Benefits will be portable across the country.
- Around 85% of rural families and 60% of urban families have already been identified.
- Launched on 25 September 2018 – on the birth anniversary of Pandit Deendayal Upadhyay.
Key Milestones in PMJAY Implementation
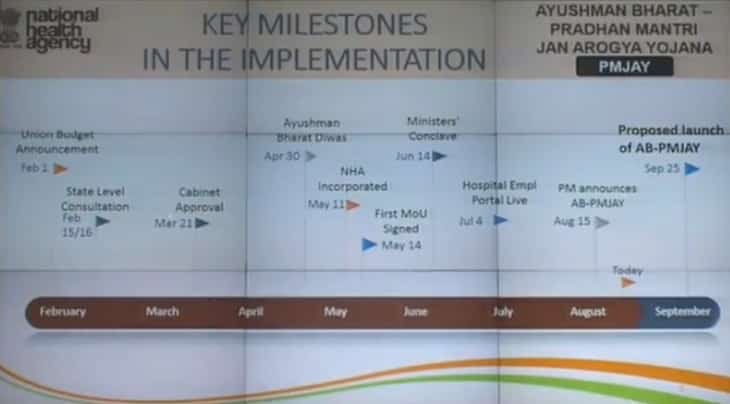
Here we are providing you the key milestones in the PMJAY Implementation:-
— It was announced on 1 February 2018 in Union Budget 2018.
— State Level Consultation was held on 15 Feb and 16 February 2018.
— Cabinet Approves Ayushman Bharat Yojana on 21 March 2018.
— Ayushman Bharat Diwas – Starting Date of Beneficiary Identification) on 30 April 2018.
— National Health Agency (NHA) incorporated on 11 May 2018.
— First MoU was signed on 14 May 2018.
— Ministers Conclave was held on 14 June 2018.
— Hospital Empanelment Portal was live on 4 July 2018.
— Pradhan Mantri Jan Arogya Yojana (PMJAY) was announced on 15 August 2018.
— Launch of Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana is on 25 September 2018.
AB-PMJAY Modes of Implementation
State can choose in which mode they want to implement this Ayushman Bharat – Pradhan mantri Jan Arogya Yojana (AB-PMJAY). There are 3 modes – Insurance Mode, Trust Mode and Mixed Mode. The name of the states along with the PMJAY mode of implementation chosen is shown below:-
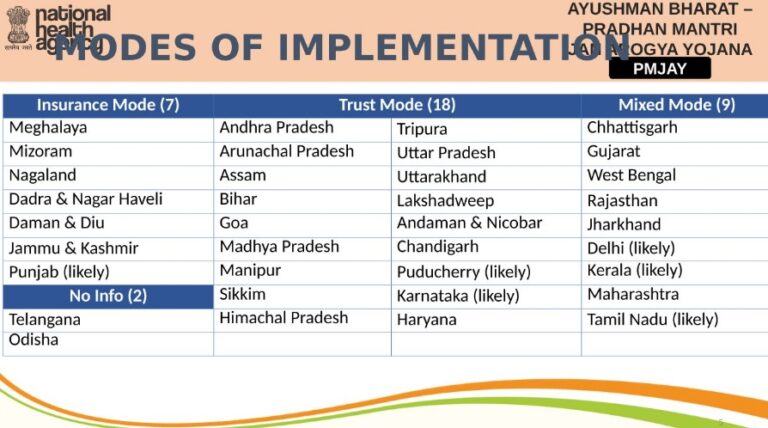
7 states have choosen to implement this AB-PMJAY Scheme in Insurance Mode, 18 in Trust Mode, 9 in Mixed Mode and 2 states have still not decided.
Strict Action Against Fake PMJAY Websites
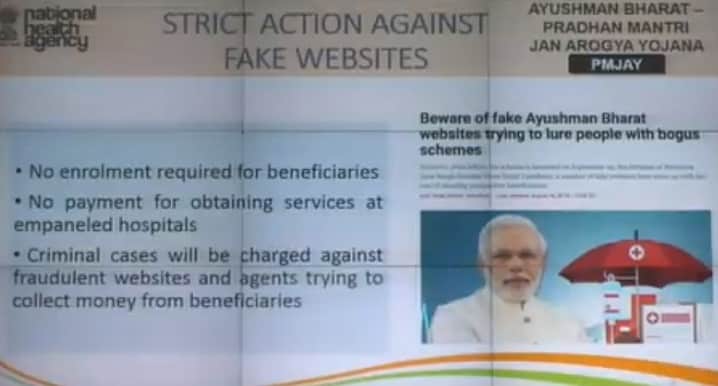
All the people should clearly note the following points regarding Ayushman Bharat – PMJAY:-
- No enrollment is required for beneficiaries to avail benefits of National Health Protection Scheme.
- He / She must not make any payment to obtain services at empanelled hospitals.
- Criminal cases will be charged at fraudulent websites and agents trying to collect money from the beneficiaries.
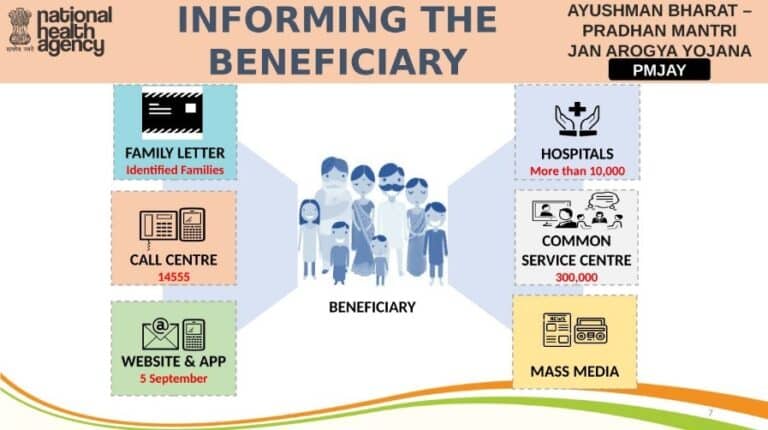
Informing the Pradhan Mantri Jan Arogya Yojana Beneficiaries
The complete procedure to inform the Pradhan Mantri Jan Arogya Yojana Beneficiaries is given below:-
- Family letter would be given to the Identified families.
- Call Centre “14555” will be open for the Pradhan Mantri Jan Arogya Yojana beneficiaries.
- Website and App was launched on 5 September 2018.
- People can get info. on Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana through 10,000 hospitals, 3 lakh Common Service Centers and by Mass Media.
Candidates can also check their name in PM Jan Arogya Yojana list of beneficiaries at mera.pmjay.gov.in
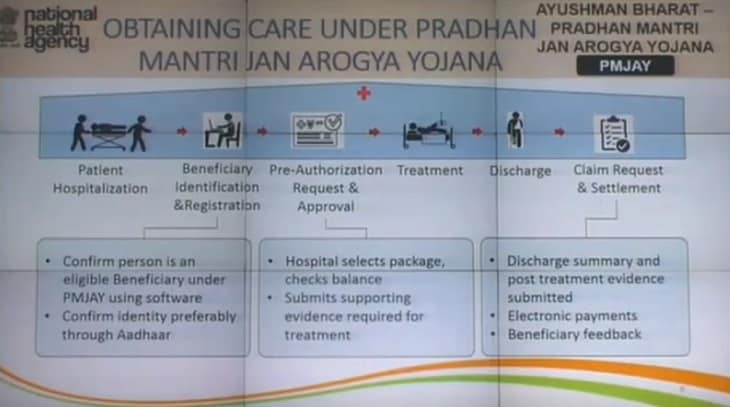
Obtaining Care under Pradhan Mantri Jan Arogya Yojana
The following steps would be followed to obtain care under Pradhan Mantri Jan Arogya Yojana:-
— Patient Hospitalization – Firstly, the hospitalization of Patients would be done.
— Beneficiary Identification & Registration – To confirm person is an eligible beneficiary under PMJAY using software. Moreover, confirmation of identity preferably through Aadhaar.
— Pre-Authorization Request & Approval – Hospitals will select package and will check balance in the card. Then they will submit the supporting evidences necessary for treatment.
— Treatment – Then patient would be given appropriate treatment.
— Discharge – After appropriate treatment, discharge would be given to the patients.
— Claim Request & Settlement – Discharge summary and post treatment evidence would be submitted. Electronics payment would be made by the govt. to the banks. After getting treatment, hospitals will ask for feedback from the patients.
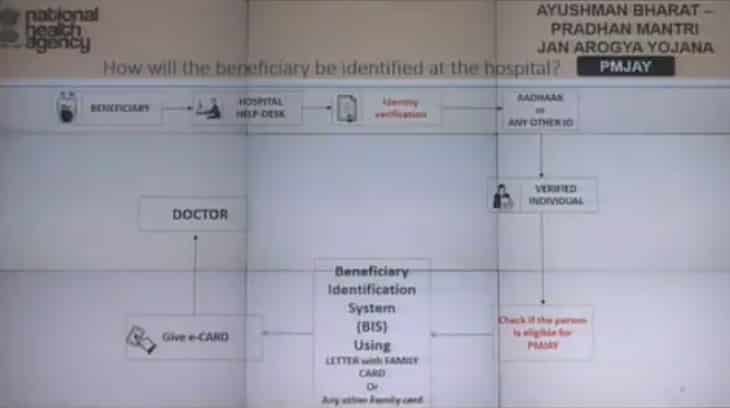
How will the Ayushman Bharat-PMJAY Beneficiary be Identified at the Hospital
Firstly Beneficiary will have to Hospital Help-Desk at which Identity verification needs to be done. For this, Aadhaar Card or an other ID needs to be provided. Next, the individual will be verified and it will be checked whether he / she is eligible or not. For this, A Beneficiary Identification System (BIS) using letter with family card. Then e-card will be given to the beneficiaries and shown to doctor for treatment.
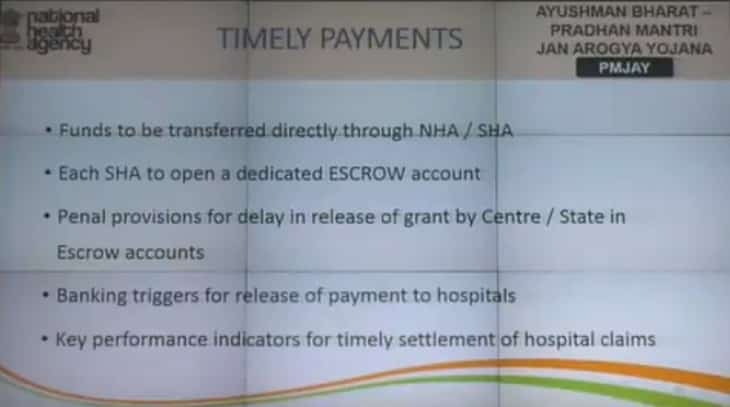
Timely Payments for Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana
All the hospitals will be ensured timely payments for treatment. Timely payments are ensured and will be done as follows:-
- Funds to be transferred directly through National Health Agency (NHA) / State Health Agency (SHA).
- Each SHA will have to open a dedicated ESCROW account.
- There are penal provisions for delay in release of grant by Center / State in ESCROW Accounts.
- Banking triggers for release of payments to hospitals.
- Key Performance Indicators for timely settlement of hospital claims.
Anti Fraud Guidelines for AB-Pradhan Mantri Jan Arogya Yojana
NHA Methodolog for Guidelines has been released now. This includes Prevention, Detection and Deterrence. Prevention will include Beneficiary Identification, Provider Emapanelment and Pre-Authorization. Detection will include Data Analytics, Social Monitoring, Audits etc. Deterrence will include Contract Management, Anti-Fraud Cells and De-empanelment & exemplary penalties.
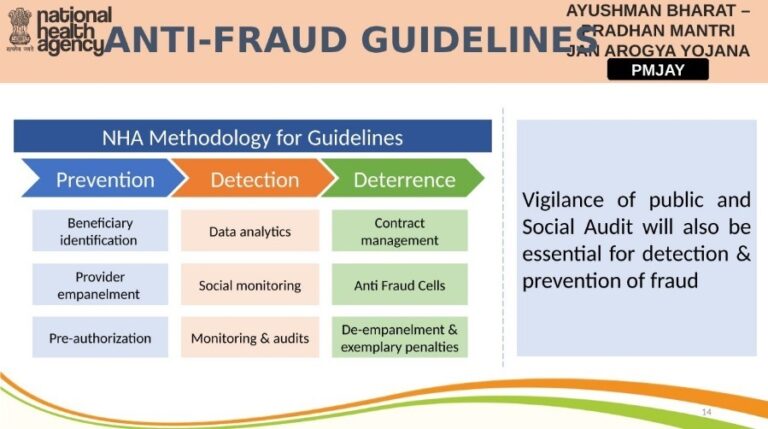
Vigilance of public and social audit will also be essential for detection and prevention of fraud.
NHA Information Security & Data Privacy Policy
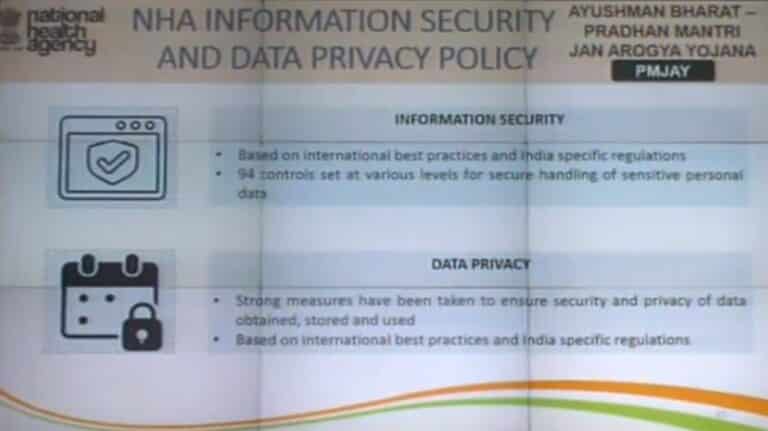
Information policy would be based on international best practices and India specific regulations. 94 controls set at various levels for secure handling of sensitive personal data. Strong measures have been taken to ensure and obtain, store and use Data Privacy. It would be based on International best practices and India specific regulations.
Pradhan Mantri Jan Arogya Yojana (PMJAY) Packages Rates
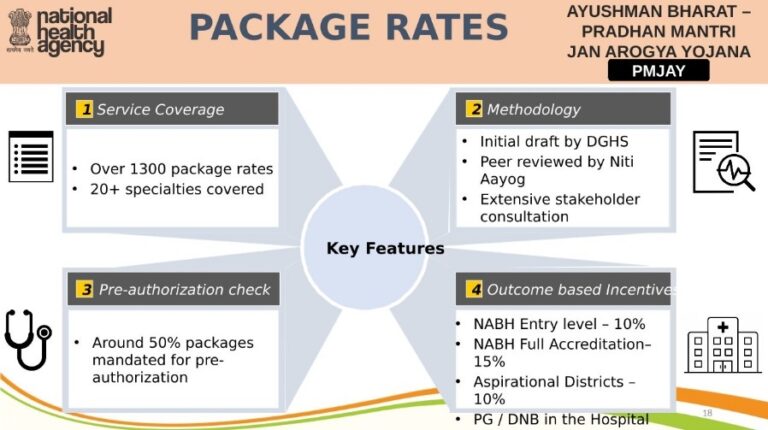
Around 1300 packages have been approved and 20+ specialities have been covered. Initial draft by DGHS, Peer reviewed by NITI Aayog and extensive stakeholder consultation. Around 50% package mandated for pre-authorization. There are outcome based incentives for hospitals like NABH Entry Hospitals to get 10% incentives, NABH Full Accrediation to get 15% incentives, Aspirational Districts to get 10% incentives.
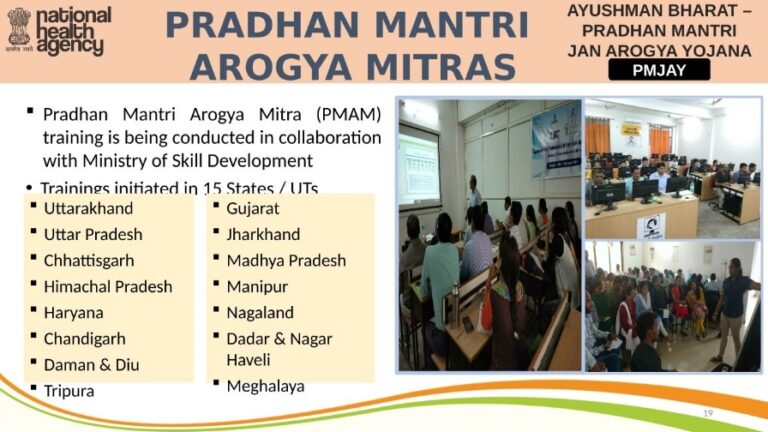
Pradhan Mantri Arogya Mitra (PMAM) Training
Pradhan Mantri Arogya Mitra (PMAM) training is being conducted in collaboration with Ministry of Skill Development. Training has been initiated in 15 States / UTs.
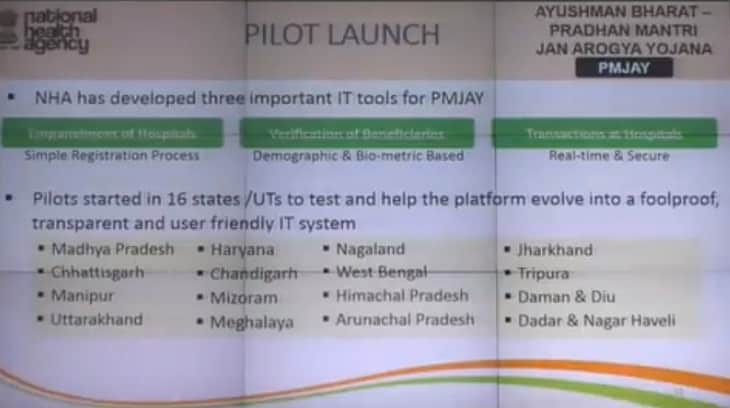
PM Jan Arogya Yojana Pilot Launch
National Health Agency (NHA) has developed 3 important IT tools for PMJAY. These includes Sinple Registration process for Hospitals Empanelment, Demographic & Bio-metric based verification of beneficiaries, Real Time & Secure Transactions at hospitals. Pilot project was started in 16 States / UTs to test and help the platform to evolve a foolproof, transparent and user friendly IT system.
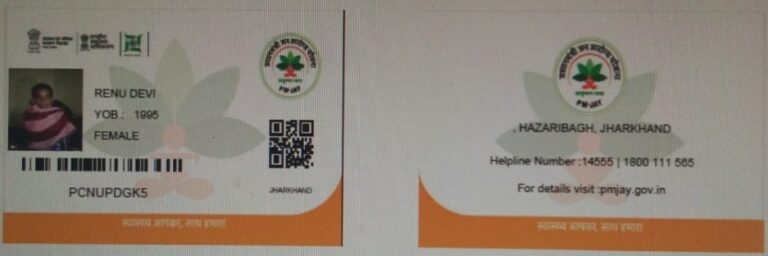
PM Jan Arogya Yojana Golden Cards – Ayushman Bharat Golden Cards
Beneficiaries are entitled to get Golden Cards to avail treatment in any govt. / private empanelled hospitals. This golden card will appear as follows:-
The government’s ambitious Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana, that will pay up to Rs five lakh in hospitalisation costs to poor and vulnerable families, will also cover drugs and diagnostic expenses three days prior to and 15 days post hospitalisation.
All Latest Updates on Ayushman Bharat Yojana (Date Wise)
Here are all of the latest updates on Ayushman Bharat Yojana in a date wise manner. The language of writing is as of the update date:-
Ayushman Bharat Scheme Hospital Empanelment Online Application Form (Update on 11 April 2020)
Central government is now inviting online application forms for Hospital Empanelment under the Ayushman Bharat Yojana. The formal express process to empanel hospitals through registration has now begun for all private hospitals to tackle COVID-19 (Coronavirus). Any hospitals can fill the Hospital Empanelment Online Application Form for enrollment under Prime Minister Rashtriya Swasthya Suraksha Mission (PMRSSM) at pmjay.gov.in
Pradhan Mantri Jan Arogya Yojana (PMJAY) will provide health protection to 10.74 crore poor & deprived rural families. Under this Modicare scheme, govt. will provide cashless and paperless benefits of upto Rs. 5 lakh to poor people in any government / private empanelled hospital with no restriction on age, family size and gender.
Check Pradhan Mantri Jan Arogya Yojana Hospitals List to find Ayushman Bharat empanelled hospitals. There is no pre-condition for treatment and people can get health benefits only through a single prescribed ID. Govt. wants that if “Illness does not consider any economic background then neither should the cure.
PMJAY Hospital Empanelment Online Application Form for Ayushman Bharat Scheme
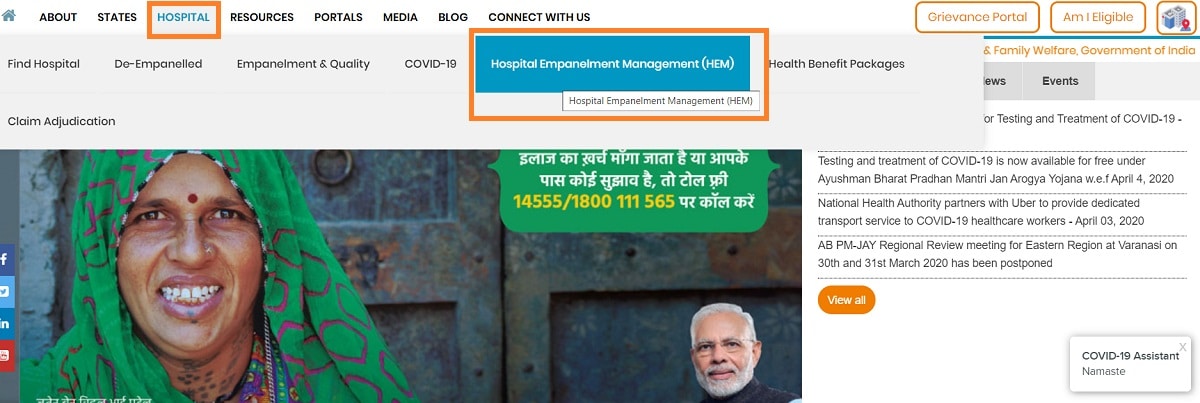
The complete procedure for hospitals to fill Hospital Empanelment Online Application Form for National Health Protection Scheme (NHPS) is given below:-
- Firstly visit the official website pmjay.gov.in
- On the homepage, click at the “Hospital” tab and then click at the “Hospital Empanelment Management (HEM)” tab as in the image:
https://ift.tt/3CBQnPo
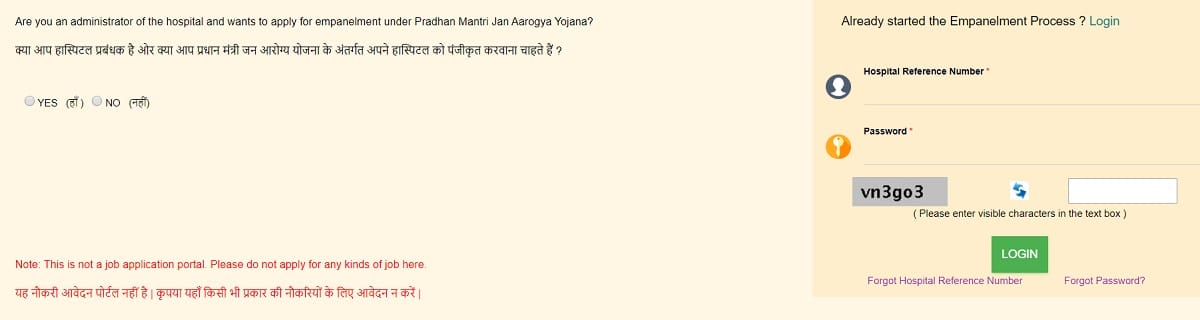
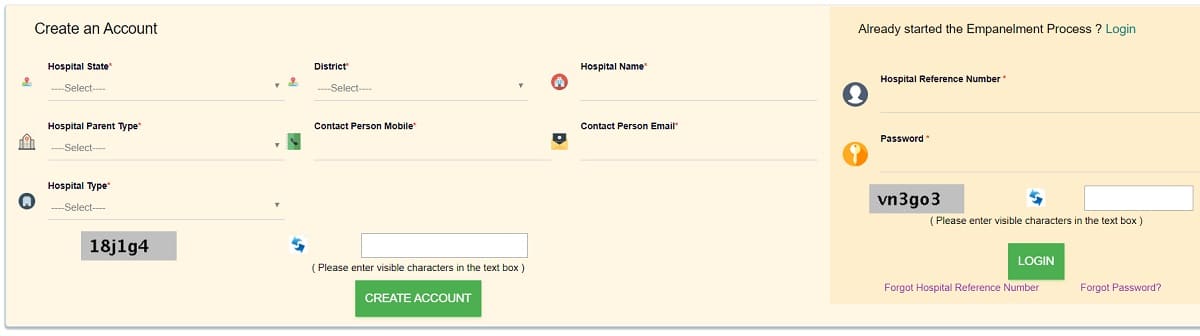
Hospitals must also check the empanelment criteria before making registration and subsequent login. Hospital’s Empanelled under RSBY need not register again. Hospitals can make ‘Login’ using Hospital Reference Number as RSBY Hospital Code as printed on your MHC and Password as Hospital’s PIN Code.
Ayushman Bharat Yojana Benefits
The new National Health protection Scheme will ensure the following benefits to the beneficiaries:-
- An Insurance Cover of 5 Lakh Per Family Per Year.
- No Restriction on Family Size, Age or Gender.
- All Eligible Family Members whose name appears in SECC Database / Ayushman Bharat Yojana Rural & Urban List of Beneficiaries are automatically covered.
- Beneficiaries need not pay any money for the treatment in case of hospitalization.
- From 1st day of policy, pre-existing conditions will be covered. These benefits will also include pre and post hospitalization processes.
- People can get treatment in any public / private / private empaneled hospitals.
- People must carry a prescribed ID to get treatment at the hospital.
Hospital Empanelment Query – For any support, please contact +918860003730 during working hours.
NHA Express Private Hospital Empanelment under Ayushman Bharat Yojana
National Health Authority (NHA) launches express empanelment to bring large number of private hospitals under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY). This empanellment of private hospitals will ensure continued essential treatment for serious illnesses like cancer and heart ailments. This decision is taken after recent one of bringing testing and treatment of COVID-19 under AB-PMJAY scheme. The treatment of Coronavirus would be carried out as per protocols and guidelines of ICMR.
In the current Novel Coronavirus (COVID-19) outbreak, several medical colleges, civil hospitals and district hospitals are being converted as dedicated COVID-19 facilities. So Hospital Empanelment Module (HEM) Lite is launched for patients suffering from serious illnesses, such as cancer, cardiac issues and diabetes. All such patients requires continuous treatment and will be able to continue getting inpatient services without the fear of contracting the COVID-19 infection.
This express private hospital empanelment under Ayushman Bharat Yojana mechanism will help in empaneling dedicated COVID-19 hospitals as well. Hospitals can empanel themselves for a temporary period of 3 months through a simpler, user friendly online system available on the scheme website www.pmjay.gov.in.
Treatment For Serious Illnesses in Ayushman Bharat PM-JAY
In order to ensure treatment of AB-PMJAY patients doesn’t suffer as many currently empaneled hospitals are converting themselves to dedicated COVID-19-only facilities. To increase our capacity to serve beneficiaries of PMJAY Scheme, the central govt. has started express empanelment of private hospitals on a temporary basis. Govt. is reaching out to states, hospital associations and healthcare industry bodies with this new proposal. The new mechanism will onboard private hospitals through a simple, quick and seamless system on a temporary basis.
All such hospitals have the choice whether to provide regular treatment for serious illnesses such as cancer and cardiac illnesses under the scheme. Moreover, these hospitals can even convert themselves into COVID-19 only hospitals providing dedicated testing and treatment to COVID-19 patients.
Timeline of PMJAY Hospital Empanelment on HEM Lite
Using the HEM Lite, will take less than 1 hour for a hospital to fill the application form along with documents. Hospital Empanelment Management (HEM) is built in a way to ensure that the process of approval by concerned authorities is expeditious. For your easy reference, an empanelment guidebook has also been provided. In case hospitals get stuck anywhere, they can call the NHA representative for prompt response and extend full support on submission of the form.
The scheme covers more than 1500 health benefit packages of procedures pertaining to secondary and tertiary care and hospitals are reimbursed at pre-fixed rates. The package prices are revised periodically and new rates were launched last year. Over and above listed price, there is further incentive available to hospitals up to 39 per cent (cumulative) for NABH entry level/full accreditation, geographical location (metro/aspirational districts) and for running PG courses.
As on date more than 8,804 private hospitals are empaneled under AB PM-JAY across the country and account for 51% of all treatments (96 lakh hospitalisations) and 64% of the hospital admissions amount (Rs 13,000 crore). The claim money is transferred within 15 days from date of submission of documents by hospital and there is a robust system for grievance redressal.
Free Novel Coronavirus (COVID 19) Treatment / Testing in Ayushman Bharat (PMJAY) Scheme (Update on 4 April 2020)
Central govt. has started free treatment and testing for Novel Coronavirus Symptoms under Ayushman Bharat Scheme 2020. All those people who shows symptoms like pneumonia, fever, difficulty in respiration can now go for free checkups. The COVID 19 complete treatment would also be provided to the infected person under PM Jan Arogyua Yojana. This free treatment of symptoms of Coronavirus disease shall remain available through different packages of Ayushman Bharat PMJAY for beneficiaries.
All the people suffering from COVID 19 disease can now avail free treatment, testing and checkup facility at private labs, govt. hospitals, empanelled private and other designated hospitals. National Health Authority (NHA) will be the nodal agency to provide treatment to COVID 19 infected persons. More than 50 crore people would now be eligible for COVID-19 Treatment / Testing under Ayushman Bharat Health Insurance scheme.
In case you have fever, cough and difficult breathing, call state helpline number or central govt’s control room 011-23978046.
Free Coronavirus (COVID-19) Treatment / Testing in Ayushman Bharat Yojana
The symptoms for which free treatment is available under Ayushman Bharat-PMJAY includes pneumonia, fever and respiratory failure. Testing and treatment of COVID-19 is already available for free in public facilities. Now, more than 50 crore citizens, eligible under the health assurance scheme will be able to avail free testing through private labs and treatment for COVID-19 in empanelled hospitals. An official of the central govt. tweeted “Treatment of symptoms of #COVID19 #Corona like Pneumonia, Fever, Respiratory Failure etc. is available, thru diff. Packages, under #AyushmanBharat #PMJAY free of cost for eligible people in empanelled hospitals & other designated hospitals.”
Central govt’s flagship Ayushman Bharat PM Jan Arogya Yojana (AB-PMJAY) provides insurance coverage of upto Rs. 5 lakh per annum per family per year. This health insurance facility is for secondary and tertiary care hospitalization to more than 10.74 crore poor and vulnerable families across the country. All AB-PMJAY Beneficiaries are entitled to get cashless and paperless access to serviceshand rub at empanelled and designated hospitals.
Till date, there are 1,578 health benefit packages with defined rates under PM-JAY and over 20,761 public and private hospitals across the country have been empanelled. Check Ayushman Bharat Yojana Package Rates. Currently, the central govt. has issued 12.41 crore e-cards to AB-PMJAY beneficiaries. Moreover according to NHA, 91.70 lakh hospital admissions have taken place under the scheme.
The COVID-19 tests will be carried out as per protocols of the Indian Council for Medical Research (ICMR) and by private labs approved or registered by it. Health experts said that social distancing and extensive testing are the only two most potent weapons in the fight against the highly contagious Coronavirus. This COVID-19 virus has infected over a million people across the world. While the centre is strictly enforcing the nationwide lockdown to stem the spread of the virus, the country has one of the lowest testing rates among the affected nations.
To bolster coronavirus testing numbers, the centre has recruited several private labs. However, there were concerns that poor people will not be able to afford them as the cost is steep – Rs 4,500 per test. Active private sector involvement will be critical in case there is a surge in the number of COVID-19 patient that need care. States are in the process of enlisting private sector hospitals that can be converted to COVID-19 ONLY hospitals,” the NHA added.
Protective Measures Against Novel Coronavirus (COVID 19)
People can now take the following protective measures against coronavirus:-
- Wash your hands with soap and water frequently.
- Use Alcohol based hand rub.
- Avoid touching your eyes, nose and mouth.
- Maintain Social Distancing.
- Avoid organizing and participating in large groups.
- Cover your mouth while sneezing and coughing.
- Don’t spit in public.
- Avoid close contact if you are experiencing cough or fever.
Coronavirus cases in India
The number of positive coronavirus cases in India has been raised to 2,301 (56 deaths) by 4 April 2020. NHA has issued advisory to consult designated hospitals in case of any COVID-19 symptoms. All the hospitals are fully equipped with treatment, testing and isolation facilities. NHA has also issued a toll-free support number:- 1075 or 1800-112-545. Since this disease is infecting health of citizens of more than 100 countries, so the World Health Organization (WHO) has declared Novel Coronavirus (COVID 19) as pandemic.
Ayushman Bharat Yojana (PM-JAY) Health Benefits Packages 2.0 & Rates (Update on 11 March 2020)
Central govt. has released Ayushman Bharat Yojana (PM Jan Arogya Yojana) Treatment List in Health Benefit Packages 2.0 and their rates. Various status such as Uttar Pradesh has already implemented Health Benefit Packages 2.0 under Ayushman Bharat PMJAY. Accordingly, UP is the 1st of the 5 states to implement HBP 2.0. A pilot project of the new health benefit package was earlier completed in Nagaland after which several states became interested in implementing it. There are more than 1578 procedures in Health Benefit Package 2.0.
In order to remove duplication, various cross specialty packages have been introduced the new benefit package. In HBP 2.0, there are 554 packages which have been discontinued and 237 packages have been added. In HBP 1.0, there are 1393 treatment packages out of which 1083 are surgical, 309 medical and 1 unspecified packages.
Accordingly, HBP 2.0 of the Ayushman Bharat Yojana has 872 treatment packages with 1,578 procedures. Out of these, 612 surgical packages have 1052 procedures while 260 medical packages have 526 treatments.
Ayushman Bharat PMJAY Health Benefit Packages (2.0) and Rates List
People can now check the full list of specialists / treatments and their rates under Ayushman Bharat-PMJAY HBP 2.0. This can be checked on the official PMAY website (www.pmjay.gov.in) or by visiting this link:-
https://ift.tt/3ETqFGq
Ayushman Bharat – PMJAY provides health insurance cover of upto Rs. 5 lakh per family per year. This amount would be given for secondary and tertiary care hospitalization to more than 10.74 crore poor and vulnerable families. Under PM Jan Arogya Yojana, govt. will provide cashless and paperless access to services are provided to the beneficiaries at the point of service.
Till date, there are over 20,761 public and private hospitals which have been empanelled across the country to provide in-patient services to the beneficiaries. As per the National Health Authority (NHA), more than 88 lakh cases of hospital admissions worth Rs. 12,169 cr have been authorized under the scheme. NHA is the nodal agency for the implementation of the AB-PMJAY scheme.
51 lakh Ayushman Bharat Beneficiaries in Bihar
Till March 2020, the implementation of Ayushman Bharat Yojana in Bihar has crossed a major milestone. As many as 51 lakh beneficiaries had received their Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) e-cards. There are e-cards has been issued to over 24.19 lakh families. These are 22% of the eligible families of Pradhan Mantri Jan Arogya Yojana in the state.
Ayushman Bharat Health Benefit Packages Revision – 237 HBP Added, Rates of 270 Hiked (Update on 28 September 2019)
National Health Authority (NHA) has revised the Ayushman Bharat Health Benefit Packages. NHA has added 237 new packages in the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY). The rates of 270 Health Benefit Packages (HBP) has been raised, 43 stratified packages have been adopted while there is no change in rates of 469 packages.
NHA said that the revision in the HBP packages will not affect the range of treatment covered under PM Jan Arogya Yojana. Without comprising range of treatment covered under AB-PMJAY scheme, around 554 packages would be discontinued while there is reduction in rate of 57 packages.
This reduction in Ayushman Bharat Health Benefit Packages will reduce abuses of packages by fraudsters at different level.
Ayushman Bharat Health Benefit Packages Revision
The revision of Health Benefit Packages (HBP) of Ayushman Bharat Scheme will motivate more private hospitals to join the PMJAY scheme. People can now check the HBP packages revision in the table below:-
| Rates After AB-HBP Revision | Number of Packages |
|---|---|
| Increase in Rates | 270 Packages |
| Adopted | 43 Packages |
| No Change | 469 Packages |
| Reduction in Rates | 57 Packages |
| Discontinued | 554 Packages |
| Newly Added | 237 Packages |
NHA has made an attempt to keep prices of abuse prone packages at minimum level to minimize incentives for abuse. With revision in Ayushman Bharat health benefit packages, many new private hospitals will get empanelled with PMJAY scheme. This is going to improve the access to good quality healthcare and lakhs of vulnerable families will receive free treatment.
Packages under Ayushman Bharat
PMJAY health insurance scheme is offering 1,393 treatment packages for cashless and paperless treatment. Out of these, 1,083 packages are surgical, 309 medical and one unspecified package. These AB health benefit packages includes cost of diagnostics upto 3 days before hospitalization and medicines upto 15 days post-hospitalization. NHA is consistently receiving feedback on various aspects of PMJAY scheme which includes existing HBP and their rates.
Before finalizing the changes in Health Benefit Packages, feedback was also taken from the States and Union Territories. Their feedback was examined by the review committee setup for Ayushman Bharat – PM Jan Arogya Yojana.
All the states & UTs which are implementing AB-PMJAY scheme using insurance model or combination of trust and insurance model will have autonomy on this decision. They can continue implementing Ayushman Bharat Yojana using existing package master till their current contract period ends or can shift to the new version after making suitable amendments in their contract.
Cancer Care Revamp in Ayushman Bharat HBP Revision
The revised oncology packages of Ayushman Bharat Scheme will revamp cancer care for beneficiaries. This will align to reflect current best practices in the country. The revised HBP rates will further augment cancer care in the country with reduction in catastrophic expenses associated with its treatment.
After AB-HBP revision, oncology packages have been split to include multiple regimens of surgical and medical oncology complemented by radiotherapy regimens. This will standardize the nomenclature and definitions of packages. NHA in collaboration with World Health Organization (WHO) has started process of aligning HBP with International Classification of Health Interventions (ICHI) and International Classification of Diseases (ICD) coding of the WHO. On completion, India will become first country to use ICHI in HBP list.
Ayushman Bharat Scheme – Addressing Price Movement
NHA is also planning to configure the cost of implants / high-end consumables in its IT system separately at the backend. This would be useful in case there is a movement in the price of these significant components of a package cost.
Ayushman Bharat (PM-JAY) Mobile App Download [PM Jan Arogya Yojana App] (Update on 8 Feb 2019)
Central government has launched mobile application for Ayushman Bharat Scheme or Pradhan Mantri Jan Arogya Yojana for smartphone users. Now all the people can download Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) app from the google playstore. National Health Authority has developed Ayushman Bharat (PM-JAY) mobile app which is of 4.52 MB size and is currently available for android users.
PM-JAY is a flagship scheme of the Modi govt. to provide cashless secondary and tertiary care treatment from the empanelled public and private hospitals. AB-PMJAY scheme provides coverage to more than 10 crore poor and vulnerable beneficiary families.
This PM-JAY mobile app has already recorded over 10,000 installations in the 2 days. AB-PMJAY App offers easy access to information on the scheme and will allow them to check eligibility, find nearby hospitals and receive help.
Ayushman Bharat (PM-JAY) Mobile App Download
In the recent Union Budget 2019-20, the state govt. has allocated Rs. 6400 crore for Mega Health Insurance Scheme named Ayushman Bharat – PM Jan Arogya Yojana. National Health Authority (NHA) is the apex body responsible for the implementation of Ayushman Bharat PM-JAY. NHA has now developed Ayushman Bharat (PM-JAY) mobile app which is available to download at google playstore for android users. The official link to download ayushman bharat mobile app is given here – PM Jan Arogya Yojana App Download
Users can even check their wallet at this PM-JAY mobile app of Ayushman Bharat Scheme. This AB-PMJAY app will display how much money has been used and people can also register their grievances here. This PM Jan Arogya Yojana mobile app was under testing for the last few days and has already reached 10,460 downloads and the central govt. expects this number to touch a lakh.
Ayushman Bharat Yojana was launched by PM Narendra Modi on 23 September 2018 from Jharkhand. PM Jan Arogya Yojana is going to benefit around 55 crore people and will provide Rs. 5 lakh for secondary and tertiary care hospitalization through a network of Empanelled Health Care Providers (EHCP).
Facts on PM Jan Arogya Yojana (AB-PMJAY)
Till date, 10.33 lakh beneficiaries have been hospitalized and claims worth Rs. 1041.3 crore have been settled out of which around Rs. 808.2 crore has already been approved. Moreover, around 60,328 hospitals have applied for empanelment and out of which 14,434 (24.40%) have been empanelled till now. Moreover, govt. has issued 4.63 lakh more cards, so the total number of cards now reaches 1.28 crore.
In total, the overall Indian healthcare market currently stands at $100 Bn as per IBEF and is going to touch $280 Bn by 2020 which is growing at a CAGR of 22.9%. For more details, visit the official website at pmjay.gov.in
Benefits of Ayushman Bharat – PM Jan Arogya Yojana App (AB-PMJAY App)
This Ayushman Bharat (PM-JAY) app would also address the issue of rise in fraudulent apps which lure smartphone users and redirect them to pay with false promises of enrollment in the PM Jan Arogya Scheme. People would be able to get access to all information related to PM Jan Arogya Yojana. Moreover, people can easily check eligibility and can even search empanelled hospitals.
Google has given assurance that after the launch of this AB-PMJAY mobile app, this app will now figure at the top of the list through search engine optimization. Around 28 states and union territories are on board currently with the scheme.
How to Get Job as Ayushman Bharat Arogya Mitra – Eligibility Criteria & Details (Update on 26 November 2018)
Central govt. has started Ayushman Bharat Yojana across the country and it has created jobs for around 1,00,000 Arogya Mitras in empanelled hospitals. How to get Arogya Mitra Job under Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) mega health insurance scheme is the most frequently asked question now a days. People can check the eligibility criteria, recruitment process, guidelines and apply for Ayushman Mitra vacancy with Rs. 15,000 salary at the empanelled hospitals.
Ayushman signifies “long life” and thus Ayushman Bharat scheme aims to provide long life to all Indians. Ayushman Bharat Yojana enables people to avail cashless and paperless treatment in any of the public or private empanelled hospitals. This scheme aims to provide Rs. 5 lakh health insurance to around 50 crore poor people for secondary and tertiary hospitalization. Arogya Mitras are an essential part of implementation of Ayushman Bharat Yojana.
Now check the eligibility criteria, roles and responsibilities, salary, recruitment process and other details regarding Arogya Mitras in this post.
Ayushman Bharat Arogya Mitra Job / Salary
Beneficiaries can check their names, go to any of the PMJAY empanelled hospital carrying their one identity proof (ration card or voter card or ayushman family card or aadhaar card) to verify their identity and can avail cashless treatment. After going to the hospitals, people can meet the person at the helpdesk which is named as Arogya Mitra. These Arogya Mitras are specially appointed persons who are present in every empanelled hospitals to assist people in getting cashless and paperless treatment. These employees have complete knowledge about the Ayushman Bharat Yojana, treatment procedures, package rates and also helps people in their claim settlement process.
While launching the scheme, the central govt. has focused on designing a support system to assist beneficiaries at Empanelled Health Care Provider (EHCP). To streamline the entire process of health service delivery and provide a seamless experience to the Ayushman Bharat Yojana beneficiaries, Arogya Mitra have been placed at each EHCP. We must tell you that all those people who are interested in becoming an Arogya Mitra with Rs. 15,000 salary can directly contact the empanelled hospitals under the Ayushman Bharat Scheme in which they want to get a job and assist people.
Arogya Mitra Eligibility Criteria
An Arogya Mitra / Ayushman Mitra (AM) is a certified frontline health service professional who shall be present at each of the EHCP and shall serve as a first contact point for beneficiaries. Below is the complete eligibility criteria to get selected as an Arogya Mitra:-
- He / She must have completed 12th (10+2) from a recognized institution.
- Candidate must possess basic proficiency in computer operations.
- Must have completed Ayushman Mitra Training Course and passed the respective course exam / certification.
- Candidates must possess fluent communication skills in Hindi / English and local language of the state or region.
- Applicant must have adequate functional computer literacy which includes understanding of Microsoft Office Suite and navigating through internet portals.
The central govt. has made a provision in which preference will be given to the female candidates for the position of Ayushman Mitra. All the qualified ASHA workers may be given preference for the position of AM. The existing staff of govt. hospitals can also be nominated to act as Ayushman Mitra by the state government.
Who will Carry Recruitment Drive for Ayushman Bharat Arogya Mitra
Here we will give you the information about the agencies who will carry out the recruitment drive for Arogya Mitras:-
- The State Health Agency (SHA) has the flexibility to recruit Arogya Mitra through 3rd party agency or any other mechanism for public facilities. The SHA will pay the salaries to the Ayushman Mitras thorugh 3rd party agencies. If extra AMs are recruited, then SHA / selected agency can scale up its capacity and provide the necessary number of AMs.
- SHA have the authority to directly hire the AMs at state / district or at hospital level.
- In case the state govt. requires more AMs, then they can even nominate the existing staff of public hospitals as AM.
- For private EHCP, the recruitment and placement of Arogya Mitra would be done by the health care provider itself. Private EHCP will have to bear the cost of AM in that facility.
AMs will be placed at every public EHCP and the exact numbers of AMs to be placed will depend on the number of average cases load in a single day. In case there are 0 to 10 cases, then 1 AM will be required. For 10 to 20 cases in single day, 2 AMs would be required, for 20 to 30 cases, 3 AMs would be required and for more than 30 cases there would be 4 AMs. An Arogya Mitra may be hired for initially a period of 1 year and their contract can be renewed yearly on the basis of performance.
Guidelines for Arogya Mitra Recruitment
All the Arogya Mitras can also check the responsibilities to be performed at the help desk / kiosk, training details and other benefits to Ayushman Mitras. To check the guidelines for recruitment of Arogya Mitra, please click the link given below:-
Guidelines for Ayushman Mitras
All the candidates must fulfill the following conditions mentioned in the guidelines before applying for this job.
List of Specialties & Specialty Codes of Treatments Covered Under PMJAY (10 Nov 2018)
The list of specialties covered and specialty codes under Pradhan Mantri Jan Arogya Yojana (PMJAY) was released by the central government just after the launch of the schemes. The complete details of the specialties codes & their name can be seen at the official website at pmjay.gov.in or mera.pmjay.gov.in. In the list of empaneled hospitals under Ayushman Bharat health insurance scheme, specialties are shown in the form of S & M codes.
All the beneficiaries of PM Jan Arogya Yojana at any empaneled hospital can check the specialty covered at that particular hospital using these specialty codes. After accessing the specialty covered, PMJAY beneficiaries can select the best hospital located nearby as per their requirements. There are a total of 24 specialties are covered under PMJAY out of which 8 have M codes and 16 have S codes.
The specialty codes are mentioned in the PMJAY list of empaneled hospitals in the extreme right column along with the hospital details like type of hospitals, address, e-mail ID & contact number. Below is the complete list of specialties covered under Ayushman Bharat health insurance scheme along with the specialty codes associated with each specialty:
PMJAY Specialty List & Codes
| S. No. | Name of Specialty | Specialty Code |
|---|---|---|
| 1. | General Medicine | M1 |
| 2. | Paediatric medical management | M2 |
| 3. | Neo-natal | M3 |
| 4. | Paediatric cancer | M4 |
| 5. | Medical oncology | M5 |
| 6. | Radiation oncology | M6 |
| 7. | Emergency room packages (care requiring less than 12 hrs stay) | M7 |
| 8. | Mental disorders package | M8 |
| 9. | General surgery | S1 |
| 10. | Otorhinolaryngology | S2 |
| 11. | Opthalmology | S3 |
| 12. | Obstetrics & gynaecology | S4 |
| 13. | Orthopaedics | S5 |
| 14. | Polytrauma | S6 |
| 15. | Urology | S7 |
| 16. | Neurosurgery | S8 |
| 17. | Interventional neuroradiology | S9 |
| 18. | Plastic and reconstructive | S10 |
| 19. | Burns management | S11 |
| 20. | Cardiology | S12 |
| 21. | Cardio-thoracic & Vascular Surgery | S13 |
| 22. | Paediatric surgery | S14 |
| 23. | Surgical oncology | S15 |
| 24. | Oral and maxillofacial surgery | S16 |
M specialty codes are numbered from 1 to 8 (M1 to M8) while S specialty codes are numbered from 1 to 16 (S1 to S16) on the basis of name of the specialties.
List of Hospitals for Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) (Update on 9 November 2018)
The list of hospitals for the Ayushman Bharat (Pradhan Mantri Jan Arogya Yojana – PMJAY) has been released by the central government. The complete list of empaneled hospitals for Ayushman Bharat – PM Jan Arogya Yojana can be checked at the official website at pmjay.gov.in or mera.pmjay.gov.in. All the eligible beneficiaries of Ayushman Bharat Yojana can check the name and contact details of hospitals to get treatment under this mega health insurance scheme.
PMJAY national health protection scheme enable around 10 crore poor families (50 crore people) to get treatment in any govt. or empaneled private hospitals. The cashless and paperless treatment at these hospitals would be given at the NHPM treatment package rates. Arogya Mitras are present at each hospital to assist people in PMJAY claim settlement without any hassle.
Everyone whose name appears in the PM Jan Arogya Yojana list of beneficiaries can get treatment anywhere in India under AB-NHPM scheme in any of the empaneled hospitals by just showing their Ayushman family card or ration card or voter card or Aadhaar card.
Ayushman Bharat List of Hospitals at abhnpm.gov.in
Below is the complete procedure to check the name, address and contact details of Ayushman Bharat hospitals in the list of empaneled hospitals for Pradhan Mantri Jan Arogya Yojana:
Step 1: Firstly visit the official website www.pmjay.gov.in
Step 2: At the homepage, click at the “List of Empanelled hospitals” link present in the main menu or directly click this link.
Step 3: Afterwards, the hospitals search page will open as shown in the figure below:
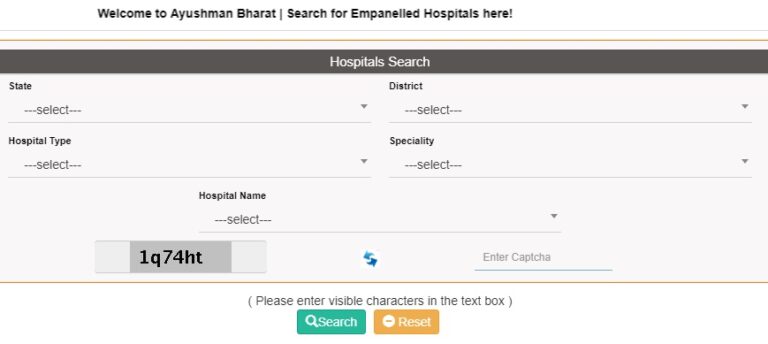
Step 4: Now select the state, district, type of hospital, specialty and hospital name and then click at the “Search” button to view the complete list of empaneled hospitals in that particular area.
Step 5: In case, you want to see the complete state-wise or district-wise list, then only select the state and or district and click the “Search” button. In the image below, we are showing you the complete list of hospitals in Faridabad district of Haryana (as a sample):
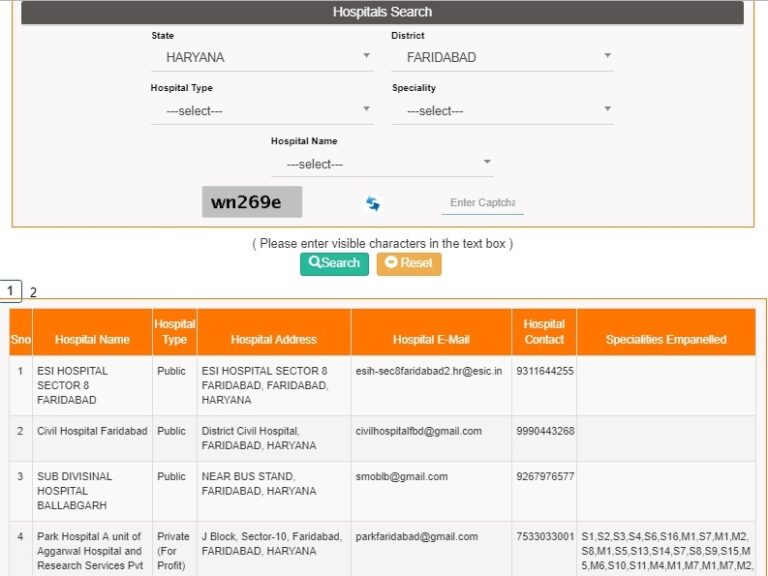
Step 6: In this list, PMJAY beneficiaries can check the type of hospital, address, e-mail ID, contact number and specialties available at various hospitals.
Check Ayushman Bharat Yojana Hospitals List at mera.pmjay.gov.in
You can also check the list of empaneled hospitals for PM Jan Arogya Yojana at mera.pmjay.gov.in for which the procedure has been described below:
- Step 1 – Firstly visit the PMJAY “Am I Eligible Portal” at mera.pmjay.gov.in.
- Step 2 – At the homepage, click at the “Search Hospitals” link present in the main menu or directly click this link.
- Step 3 – The procedure for Step 3 to Step 6 is similar to the one as we have mentioned above. Follow the same process to check the Ayushman Bharat Yojana hospitals list.
Around 1354 medical inspection and surgeries are covered under this PM Jan Arogya Yojana (PMJAY). People can simply check their name in the beneficiaries list of Ayushman Bharat Yojana. Beneficiaries can check the PMJAY eligibility criteria and must carry any one of the ID proof to avail cashless treatment in any of the listed empaneled hospitals. All the beneficiaries can check the Pradhan Mantri Jan Arogya Yojana details to become more familiar with this mega health insurance scheme.
Aadhaar Mandatory for 2nd Time Treatment – Ayushman Bharat Yojana (PMJAY) (Update on 8 October 2018)
Aadhaar card is not compulsory to avail benefits for the first time under Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) but it is now made mandatory for those seeking treatment under PMJAY scheme for the second time. This decision comes as an aftermath of the decision of Supreme Court (SC) in which SC declares aadhaar as constitutionally valid. Now aadhar card is a recognized identity proof and thus govt. makes aadhaar mandatory for 2nd time treatment under Ayushman Bharat Yojana.
If the aadhaar number is not available with the Pradhan Mantri Jan Arogya Yojana beneficiaries, then such candidates does not need to worry. Such AB-PMJAY beneficiaries can just provide documents to prove that they have enrolled for 12 digit unique identification number. This decision will ensure that only the eligible beneficiaries avail the benefits of mega National Health Protection Scheme (NHPS) and nobody is left out. This decision is in accordance with the notification of National Health Agency, which is responsible for implementing the Ayushman Bharat – PM Jan Arogya Yojana.
Aadhaar Mandatory for 2nd Time Treatment – Ayushman Bharat (PMJAY)
Central govt. has now made it compulsory to possess aadhaar number to avail benefits of heath insurance for 2nd time under AB-NHPM scheme. The official statement stated that “We are studying the Supreme Court order. Aadhaar number or at-least documents to prove that one has enrolled for 12-digit unique identity number will be mandatory to seek treatment under the scheme for the second time”. However for the first time, one can either show their aadhaar card or voter card or ration card or golden card to avail Pradhan Mantri Jan Arogya Yojana scheme benefits.
The Ayushman Bharat-National Health Protection Mission (AB-NHPM) was renamed as AB-PMJAY and was launched pan-India by the Prime Minister from Jharkhand on 23 September 2018. Till date, around 47,000 people have already availed the benefits of world’s largest health insurance scheme PM Jan Arogya Yojana. Moreover, around 92,000 people have already been given golden cards to avail treatment at NHPM package rates in govt. / private empanelled hospitals.
Under AB-PMJAY scheme, there is no restriction on the size of family, age, gender and is going to benefit 10.74 crore poor families. Under this Ayushman Bharat Yojana, govt. aims to provide Rs. 5 lakh per family per annum for secondary & tertiary hospitalization through a network of Empanelled Health Care Providers (EHCP).

The PMJAY will provide cashless and paperless access to services for the beneficiary at the point of service. The basis of selection of beneficiaries for Ayushman Bharat scheme is only deprivation rather then caste or religion or communities. This NHPS scheme includes 8.03 crore in rural areas and 2.33 crore in urban areas as per Socio-Economic Caste Census (SECC) 2011 data.
NHA official said that around 98% of the total beneficiaries have been identified. People can also check their name in the PM Jan Arogya Yojana list of beneficiaries to avail scheme benefits. Around 14,000 hospitals across the country have been empanelled for this Ayushman Bharat health insurance scheme. Till date, around 32 states and union territories have signed MoUs with the center and will implement this programme. Telangana, Odisha, Delhi and Kerala have still not signed MoUs for the implementation of this scheme.
Treatment of Child Cancer Now under PMJAY (11 September 2018)
Central govt. has decided that the treatment of Child Cancer will now be covered under Pradhan Mantri Jan Arogya Yojana. As per the statement of NITI Aayog Member Dr. Vinod Kumar Paul, govt. has already fixed the rates for childhood treatment. Dr Paul said the scheme will provide health insurance cover of five lakh rupees to poor families. He said BPL and lower-middle-class families will benefit from it. Union govt. has decided to open 1.5 lakh Health and Wellness Centres by FY 2022 under Ayushman Bharat Scheme. These HWCs will provide comprehensive healthcare against diseases like diabetes, cancer, hypertension and cardiovascular diseases.
NITI Aayog official said that childhood cancer will be available for treatment under Pradhan Mantri Jan Arogya Yojana (PMJAY). This information was shared by Vinod Kumar Paul, while attending a function in New Delhi on 9 September 2018. Central govt. has approved treatment package rates for 1350 diseases. Along with these diseases, treatment of childhood cancer will be covered under PM Jan Arogya Yojana. There is a need for inclusion of childhood cancer in AB-PMJAY Scheme due to following reasons:-
- If diagnosed at early stages, childhood cancer is curable disease.
- This disease is not infectious and doesn’t spread from 1 child to another.
- Childhood Cancer is not usually inherited through genes. Early diagnosis and prompt treatment are necessary for good cure rate.
- Cancer in children differs from adults in many ways. Children are fast growing but also sensitive to chemotherapy treatment. They have chances to revive early, so cancer treatment is a realistic and practically achievable goal.
- Extra Care of children should be taken at home to ensure treatment discipline and regularity, good hygiene and balanced nutrition.
- Cancer treatment is a complicated process, so it is advisable that children gets treatment in an experienced and specialized pediatric cancer unit.
Number of children who develop cancer is around 3% which is significantly low, cure rate is high and even the total productive life years saved after curing children is high. So, govt. plans to includes childhood cancer treatment in PM Jan Arogya Yojana (PMJAY).
Pradhan Mantri Jan Arogya Abhiyan under Ayushman Bharat Scheme Announced (Update on 15 August 2018)
PM Narendra Modi on the occasion of 72nd Independence Day celebration has announced to launch Pradhan Mantri Jan Arogya Abhiyan. This is the last speech of PM Modi before 2019 Lok Sabha elections. PM Jan Aarogya Abhiyaan will be launched under Ayushman Bharat Scheme on 23 September 2018. Ayushman Bharat – National Health Protection Mission (AB-NHPM) will boost affordable healthcare and will provide Rs. 5 Lakh as Health Insurance to around 50 crore people.
PM Narendra Modi is currently addressing the nation from Red Fort in New Delhi. It is PM Modi’s fifth and final Independence Day speech. The Prime Minister had recently sought ideas from people for his Independence Day speech. The software for Jan Arogya Yojana will be tested for the next 6 to 7 weeks and finally this scheme would be launched on the birth anniversary of Pt. Deendayal Upadhyaya (25 September).
Pradhan Mantri Jan Arogya Abhiyan Announcement
Prime Minister Modi, on the eve of celebration of 72nd Independence Day of India has announced to launch Pradhan Mantri Jan Arogya Abhiyan. This is a National Health Protection Scheme which will provide affordable healthcare facilities to poor people. To ensure transparency, the central govt. will implement this initiative through the use of technology / software.
This software is in testing process and the testing process will continue for the next 6 to 7 weeks. Afterwards, this paperless and cashless treatment facility will be available for around 50 crore people. All the families will then get Health Insurance of Rs. 5 lakh p.a under this Pradhan mantri Rashtriya Swasthya Suraksha Mission (PMRSSM). Under Pradhan Mantri Jan Aarogya Abhiyaan, all the people whose name appears in the Rural and Urban list of Ayushman Bharat Yojana Beneficiaries can avail treatment at NHPM Treatment Package Rates.
Claim Settlement guidelines are released for Pradhan Mantri Jan Arogya Abhiyan. People can make claims at all the Health and Wellness Centers, govt. hospitals and Private Empanelled hospitals. Ayushman Mitras will be enrolled to serve people and assist them during their treatment. Ayushman Family Cards will be given to beneficiaries to avail treatment benefits.
Pradhan Mantri Jan Arogya Yojana (PMJAY) Logo
The logo for Ayushman Bharat – Pradhan mantri Jan Arogya Yojana (PMJAY) has been released on 27 August 2018. It is shown in the figure below:-
Ayushman Bharat Yojana Beneficiaries Registration at Common Service Centers (CSCs) (Update on 1 August 2018)
Common Service Center (CSC) and National Health Accounts (NHA) signed an MoU to implement Ayushman Bharat Yojana through 3 lakhs CSCs. Health Ministry will support CSC Initiative on Tele-Medicines. CSCs can now register Ayushman Bharat Beneficiaries in India. National Health Protection Scheme will cover 50 crore poor people and will provide coverage of upto Rs. 5 lakh per family per year for secondary and tertiary care hospitalization.
CSCs will perform the identification and registrations of beneficiaries of Ayushman Bharat Yojana. Shri Ravi Shankar Prasad, Minister of Electronics & IT and Shri JP Nadda, Minister of Health and Family Welfare were present during the MoU signing ceremony. CSCs are now being selected for the implementation of AB-NHPM, largest healthcare scheme of world. CSCs have become major instrument of change in rural India.
Benefits of Ayushman Bharat Beneficiaries Registration at CSC Centres
All the Ayushman Bharat Beneficiaries can avail the following benefits by making registration at CSCs:-
- MoH&FW and CSC SPV are now going to implement the Ayushman Bharat Scheme through CSC centres.
- Any Beneficiary can visit their nearby located CSCs to avail benefit of this scheme.
- CSCs will help Ayushman Bharat beneficiaries for identification of their names in the MoH&FW database and their entitlement for this scheme.
- Moreover, CSCs will help beneficiaries to scan / upload their KYC documents for their identity verification and claim their entitlement.
- Beneficiaries can even print their Ayushman Family Cards through CSC Centers. This will serve as the base for their source claim.
- CSCs will spread awareness on this Ayushman Bharat Scheme and also promote it among citizens to ensure that maximum number of beneficiaries can avail this benefit.
CSCs will get Rs. 30 (tax inclusive) for assistance of beneficiary, identification, documents upload and printing a laminated card.
Ayushman Bharat Beneficiaries Registration through CSCs – Process
Below is the process which any Ayushman Bharat Beneficiary has to follow at CSCs:-
- All beneficiaries needs to visit nearby CSC centre to check their entitlement for Ayushman Bharat Yojana.
- CSC Centre will then check whether beneficiary is entitled for NHPS. CSC VLEs will upload the necessary details and documents like Aadhaar Card, Ration Card, PAN Number and others.
- Now the CSC Center will submit the details of new people for verification to the concerned approver / state authority for further verification and approval.
- MoH&FW has appointed SLA to get this application approved in particular timelines and revert it on Real Time Basis (RTS).
- CSC Center will then provide a printed card on paper to the Ayushman Beneficiaries.
- Each beneficiary can use these cards at Empanelled Hospitals to claim benefits under Ayushman Bharat Abhiyan.
These Common Service Centers (CSCs) will become a game changer in our country. People can then get treatment at NHPM Portal at specified Package Rates.
Role of Common Service Centers (CSCs) in PMRSSM
Common Service Centers (CSCs) have always played an important role in changing the life of the rural people. These CSCs have serve a great purpose in improving menstrual hygiene through Stree Swabhiman. Now with the inclusion of CSCs, the dream of Digital India is getting big leap with Ayushman Bharat Yojana.
In PM Rashtriya Swasthya Suraksha Mission (PMRSSM), 10 crore families will be benefited with this revolutionary universal healthcare scheme in India. There are around 3 lakh CSCs in 2.5 lakh Panchayat which would serve as a great help in the implementation of this scheme. These CSCs will play an impressive role in shaping new economic model for rural populations under Digital India Initiative.
1 Lakh Ayushman Mitra Jobs in PMRSSM Empaneled Hospitals – Rs. 15000 Salary (Update on 28 July 2018)
Central government is going to deploy 1 lakh Ayushman Mitra directly in Govt. / Private hospitals under Pradhan Mantri Rashtriya Swasthya Suraksha Mission (PMRSSM). Ministry of Health expects that a total number of 10 lakh jobs will be created under Ayushman Bharat – National Health Protection Mission (AB-NHPM). All the employed youths under Ayushman Bharat Yojana will get monthly salary of Rs. 15,000.
After the implementation of Ayushman Bharat Yojana, various vacancies for the posts of Doctors, Nurse, Staff, Technicians and some other posts will be created. Around 20,000 Ayushman Mitra will be deployed in the current FY 2018.
For this recruitment, Health ministry and Skill Development Ministry have made an agreement. Govt. is currently working of empanelment of 20,000 hospitals under National health Protection Scheme (NHPS). Ayushman Mitra will also receive an incentive of Rs. 50 per beneficiary.
Ayushman Mitra Works under PMRSSM
Every Ayushman Mitra will have to perform the following works under Ayushman Bharat Yojana:-
- Ayushman Mitras will have to get complete knowledge of Ayushman Bharat Portal.
- They will have to work on the software being prepared for the welfare of patients.
- To verify the identity (ID) of the selected beneficiaries using QR Code.
- To provide information of the hospital where the treatment of patients is to be carried out.
- Provide information on current status of the beneficiary to the State Agencies after discharge of patient.

All the employed candidates will have perform tasks related to the welfare of beneficiaries.
Ayushman Mitra Training Schedule
Govt. will provide training to all the Ayushman Mitra and is going to begin from the month of August 2018. For this purpose, govt. will select 1 trainee from each district and will provide them necessary training. After this, these trainees will get training at the Pradhan Mantri Skill Development Centers (Kaushal Vikas Kendras).
Ministry of Health will then conduct an examination and every candidate who have passed the exam will get Certificate. All the certificate holders will become to become Ayushman Mitra. After that, these selected candidates will be deployed as per the need of the state. Each beneficiary will also get an incentive of Rs. 50 per beneficiary.
11 Cr Ayushman Family Cards for Health Insurance under PMRSSM (Update on 18 July 2018)
Central government is going to print and hand-deliver 11 crore “Ayushman Family Cards” under Pradhan mantri Rashtriya Swasthya Suraksha Mission (PMRSSM). These cards are essential to avail cashless treatment benefits under the flagship Ayushman Bharat Yojana (Modicare). Ayushman Pakhwaras will be organized across villages to provide Health Insurance Scheme benefits to the poor rural people.
Even a new National Toll Free Number will be given to the Ayushman Bharat Yojana Beneficiaries. There will 24*7 Call Centers to attend the complaints regarding Ayushman Bharat Yojana Applications and Claim Settlement under National Health Protection Scheme. Modi Govt. has previously announced the Treatment Package Rates and to avail treatment at these rates and other HWC Services, Ayushman Family Cards will be needed. This scheme will cover 10 crore vulnerable families with 50 crore beneficiaries. Ayushman Bharat Beneficiaries can now make registration at Common Service Centers (CSCs)
Govt. is planning to complete all the preparations till 15 August 2018 but the official date of launch is still not known. Central govt. will set-up a 24*7 Call Center in the capital to attend the complaints and queries from the citizens about the scheme. Even the beneficiaries will be given assistance even if outside their home state. The salient features if these Modicare Ayushman Family Cards are as follows:-
- All the Ayushman Family Cards will contain the names of all those members who are eligible for this Ayushman Bharat Yojana.
- A personalized letter will also be attached with these Ayushman Cards describing the features of Pradhan Mantri Rashtriya Swasthya Suraksha Mission (PMRSSM).
- Central govt. has already identified around 80% beneficiaries in the Rural Areas and 60% beneficiaries in the Urban Areas.
- National Toll Free Number will be necessary to contact the Call Center which is a prerequisite for such a huge Health Insurance Scheme.
- Through these call centers, all the stakeholders will have access to seamless and timely access to information and services. Moreover, these centers will also have the facility of answering e-mails and Online Chats with the people.
- Ayushman Family Cards will help in identification of beneficiaries and other documents will be required to authenticate the information.
- Govt. is planning to print around 107 million information letters and family cards and hand deliver it to the people over the next 2 years.
- In case the families does not possess these family Health Cards, then those families will not be denied of treatment benefits.
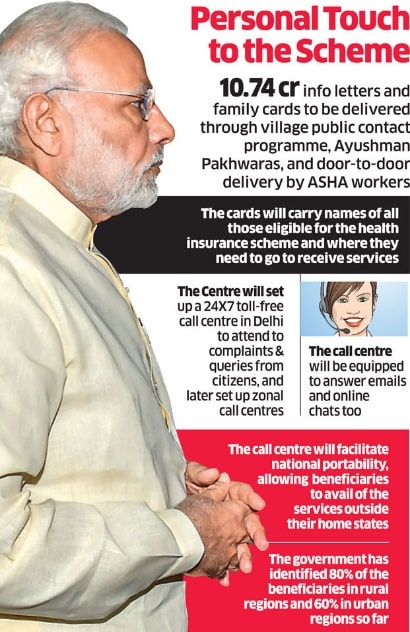
Ayushman Family Cards will reduce the uncertainty of the people whether they are eligible for PM Rashtriya Swasthya Suraksha Mission (Modicare).
Ayushman Bharat Yojana Health Cards Distribution
On getting information about the beneficiaries from National Health Agency, the Service Providers will print these Ayushman Family Cards. All the Health Cards will follow the Data Safety Standards and Right to Privacy under Modicare Scheme. Service Providers will then bundle these cards by area code and then dispatch it to the District Headquarters of beneficiaries. Then these Health Cards would be given to the Gram Panchayats and finally to the poor families through major public contact programmes.
Mass Functions will be organized like Ayushman Pakhwaras in villages and door-to-door by Health workers. Call Center Service Providers will use the Hub-and-Spoke Model and establish zonal call centres across various parts of the country. Call Centers will also facilitate the National Portability benefits of this PM Rashtriya Swasthya Suraksha Mission (PMRSSM). These call centers will possess geo-tagging capabilities and will enable govt. to serve citizens in efficient and effective ways. All the calls will be then identified on the basis of their location and will be routed to the nearest call center.
Ayushman Bharat Yojana (PMRSSM) Claim Settlement Guidelines at pmjay.gov.in (Update on 12 July 2018)
Central Government has released the guidelines for Claim Settlement under Ayushman Bharat Yojana / Pradhan Mantri Rashtriya Swasthya Suraksha Mission (PMRSSM). All Empanelled Health Care Providers (EHCP) will use an IT system of PMRSSM to manage claims related transactions. The entire process of claim registration, intimation, payment, investigation by EHCP or by Trust / Insurer is paperless.
IT system of PMRSSM will enable online transactions to ensure claim reporting in real time. However, certain districts have internet connectivity problem, so govt. included an offline arrangement in this IT system. PM Rasthriya Swasthya Suraksha Mission eliminates the need of submission of physical paper.
All the claim data will be sent electronically through IT system to the Central / State server. The NHA, SHA, Insurer (if applicable) and EHCP shall be able to access this data with respect to their respective transaction data only.
Ayushman Bharat Yojana Claim Payment and Turn-around Time
Whenever a customer raises a claim (has hit Central / State Server) under this PM Yojana, Trust / Insurance Companies must follow the guidelines for claim settlement received from EHCP:-
- Firstly, the Trust / Insurer / IRDAI Complaint Agency appointed by govt. will decide whether to accept or reject the claim received from EHCP. Rejection notice issued to EHCP must clearly state the reason for rejection as EHCP is eligible to appeal against claim rejection.
- If claim is accepted, then Trust / Insurer shall either make payment on the basis of applicable package rate or shall conduct further investigation for claim.
- Either rejection or payment / investigation must be completed in 15 days (Turn Around Time – TAT). For claims outside the State, this process must be completed within 30 calendar days. TAT will start from the date at which claim documents are accessible by Trust / Insurer.
- The EHCP should upload all claim related documents within 24 hours of discharge of beneficiary to avail benefits under PM Swasthya Suraksha Mission
- The Trust / Insurer shall make claim payments to each EHCP against payable claims on a weekly basis through electronic transfer to such EHCP’s designated bank account. Insurer will have to upload the payment details on the online portal of PMRSSM.
- Claims investigations will be undertaken by a qualified and experienced medical staff/team including at-least 1 MBBS degree holder to confirm nature of disease, illness or accident. Investigating team must not impart any treatment advice to the patients but they are allowed to verify that the medical procedure offered are upto the prescribed Standard Treatment Guidelines.
- The Trust / Insurer must also update the complete details on online PMRSSM IT system for:-
- Claims that are under investigation on a fortnightly basis for review.
- Every claim which is pending beyond TAT duration of 15 days along with reasons.
- The Trust / Insurer may collect at its own cost, complete Claim papers (including diagnostic reports) from the EHCP, (if necessary to audit claims under investigation). This shall not have any bearing on the Claim Payments to
the Empanelled Health Care Provider.
Penalty on Delay in Claim Settlement under PMRSSM
Every delay in the settlement of claims beyond TAT will invite a penalty of 1% of total claimed amount per week. This penalty amount is to given by the Trust / Insurance Companies to the hospitals. For Inter-State claims w.r.t portability of benefits, penalty will be given at 1% per week after 30 days duration.
Pradhan Mantri Rashtriya Swasthya Suraksha Mission – Update of Claim Settlement
The Trust / Insurance Company should update claim settlement data on the portal on a daily basis. After claim payment, they must update this data within 24 hours. If payment data is not updated, then it will be treated as unpaid and EHCP can levy interest on unpaid amount.
Ayushman Bharat Yojana Right to Appeal and Reopening Claims
All Empanelled Health Care Provider possess Right of Appeal against claim rejection if EHCP feels that claim is payable. All details on Right to appeal and reopening claims are present in the official notification.
PMRSSM Claim Settlement Guidelines Notification
All the details of Claim Settlement including claim registration, intimation, payment, investigation and other details are available in the notification given here – PMJAY Claim Settlement Guidelines
NHPM Portal Treatment Package Rates – Ayushman Bharat Yojana (Update on 25 May 2018)
Central Government has now approved the Treatment Package Rates of the Modicare / Ayushman Bharat Yojana. Under this National Health Protection Mission (NHPM), govt. has finalized the rate for 1,352 medical inspection and surgeries. The complete list of treatment packages for health insurance scheme will be soon available on the Portal of the Ministry and a new NHPM Portal.
National Health Protection Scheme (NHPS) will provide Rs. 5 lakh insurance cover per year to around 10 crore poor families. This will be a cashless treatment at all the govt. and private empanelled hospitals for secondary and most tertiary care procedures. Govt. is also ensuring that all the Health and Wellness Centers are working efficiently.
There is no need to fill any Ayushman Bharat Yojana Online Registration Form as this is an eligibility based scheme and there is no requirement to make any online enrollment. Till then, you can see who is eligible to take benefits through Ayushman Bharat List of Beneficiaries.
NHPM Portal Treatment Package Rate List – Ayushman Bharat Yojana
The list of Medical treatments along with the rates as fixed by the central govt. under National Health Protection Mission is given as follows:-
| Medical Treatment | Rate under NHPM |
|---|---|
| Knee Implant | Rs. 90,000 |
| Heart Stent | Rs. 40,000 |
| Bypass Surgery | Rs. 1.10 lakh |
| Replacement of Valve | Rs. 1.20 lakh |
| Arthroscopy Surgery | Rs. 20,000 |
| Hip Replacement | Rs. 90,000 |
| Knee Surgery | Rs. 25,000 |
| Cervical Surgery | Rs. 20,000 |
| Hysterectomy Surgery for Removal of Uterus (बच्चेदानी हटाने के लिए) | Rs. 50,000 |
The complete list of Treatment Packages with Rates under Ayushman Bharat Yojana will get uploaded on a new NHPM dedicated portal. In order to increase the number of Empanelled Private Hospitals under National Health Protection Scheme (NHPS), Health Ministry will also provide incentive upto 30% to private hospitals.
Under this scheme, govt. will merge Rashtriya Swasthya Bima Yojana (RSBY) and Senior Citizen Health Insurance Scheme. This scheme does not have any limitation on the income of the families and the age group of the family members. Moreover, all the diseases will be covered from the first day after Ayushman Bharat Yojana Beneficiaries Registration at CSC.
Furthermore, govt. will also provide transport allowances to the beneficiaries. All the Public / Private empanelled hospitals will get this amount directly into their account and this treatment would be cashless for all the people whose name appears in the SECC-2011 Data.
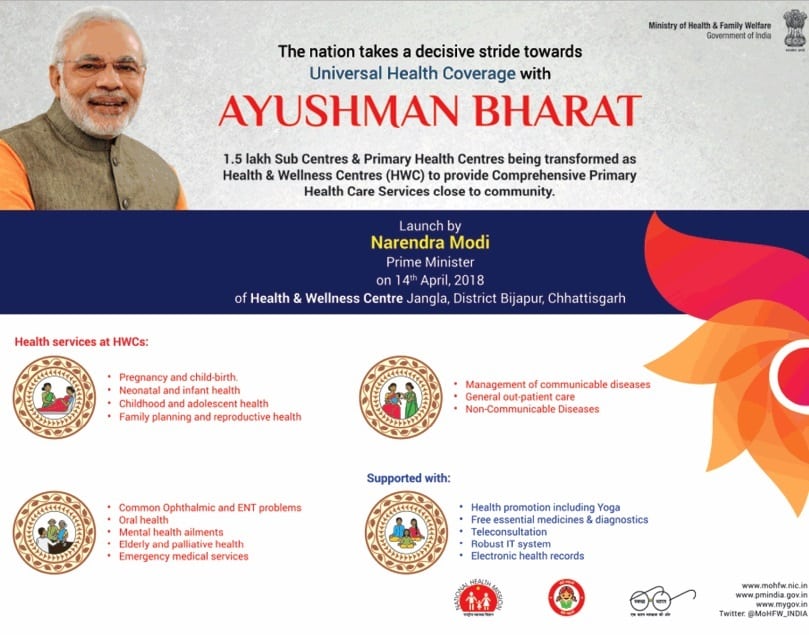
Health and Wellness Centres (HWC) Services – Ayushman Bharat Yojana (Update on 14 April 2018)
Central govt. has officially launched Ayushman Bharat Yojana 2018 as announced in Union Budget 2018-19. On Dr. B.R. Ambedkar Jayanti (14 April 2018), PM Modi inaugurates first Health and Wellness Centres (HWC) in Jangla, district Bijapur, Chhattisgarh. Under NHPS, central govt. will transform sub-centers and primary health care centers into HWC to provide comprehensive healthcare to people from below poverty line (BPL) families. See complete List of Services.
Last month, cabinet has also approved the Ayushman Bharat National Health Protection Mission (AB-NHPM). Under Universal health insurance Scheme, all the families whose name appears in the All India Final BPL List 2018 will get an insurance coverage of Rs. 5 lakh per year.
This centrally sponsored healthcare scheme is applicable for all secondary and tertiary hospitalization process in public / private empanelled hospitals. National Health Protection Scheme beneficiaries includes 10 crore bpl families and is the biggest scheme of India. See Ayushman Bharat Yojana List of Beneficiaries. Treatment Package Rates for 1352 medical inspection and surgeries are finalized by the govt. and will soon be uploaded on the NHPM Portal.
Health and Wellness Centres (HWC) – List of Services
Pradhan Mantri Narendra Modi has launched Ayushman Bharat Yojana 2018 as the nation takes decisive stride for Universal Health Coverage (UHC). Central govt. will transform around 1,50,000 Sub centers and primary health centers into Health and Wellness Centres (HWC). First HWC is opened at Jangla, dist. Bijapur, Chhattisgarh. The List of Services provided through these health & wellness centers is as follows:-
- Pregnancy and Child Birth
- Neo-Natal and Infant Health
- Childhood and Adolescent Health
- Family Planning and Reproductive Health
- Common Ophthalmic and ENT Problems
- Oral Health
- Mental Health Ailments
- Elderly and Palliative Health
- Emergency Medical Services
- Management of Communicable Diseases
- General out-patient Care
- Non-Commmunicable diseases
All the BPL families whose name appears in the Socio-Economic and Caste Census – SECC-2011 data can avail benefits.
Health and Wellness Center Features
The important features and highlights of Health and Wellness Centres are as follows:-
- Health Promotion using Yoga
- Free essential medicines
- Free diagnostics facility
- Teleconsultation
- Robust and Secure IT System
- Cashless Benefits through Health Cards
- Electronic Health Records
Cabinet Approves Ayushman Bharat – National Health Protection Mission (AB-NHPM) (Update on 22 March 2018)
Cabinet Committee of Central government has approved the launch of Ayushman Bharat National Health Protection Mission (AB-NHPM). National Health Protection Scheme has the benefit cover of Rs. 5 lakh per family per year. This Centrally sponsored scheme will cover all the secondary care and most tertiary care procedures. AB-NHPM will subsume the ongoing centrally sponsored schemes Rashtriya Swasthya Bima Yojana (RSBY) and Senior Citizen Health Insurance Scheme.
Beneficiaries will be allowed to take cashless benefits from any Public / Private empanelled hospitals. Central govt. will provide payment on Package Rate basis. Package Rates will include all the costs associated with treatment. It will be a cashless, paperless transaction for beneficiaries. See List of Services at Health and Wellness Centres.
The target beneficiaries of the proposed scheme will be more than 10 crore bpl families belonging to poor and vulnerable population based on Socio Economic Caste Census – SECC-2011 Data. See Ayushman Bharat Yojana List of Beneficiaries. Treatment Package Rates for 1352 medical inspection and surgeries are finalized by the govt. and will soon be uploaded on the NHPM Portal. Ayushman Bharat Beneficiaries can now make registration at Common Service Centers (CSCs)
Ayushman Bharat National Health Protection Mission (AB-NHPM) Features
The important features and highlights of Ayushman Bharat Programme are as follows:-
- To ensure that nobody is left out, there will be no cap on the family size and age in this scheme.
- The benefit cover will also include pre and post-hospitalization benefits.
- AB-NHPM will have a defined benefit cover of Rs. 5 Lakh per year per household.
- NHPS benefits are portable across the country.
- Beneficiaries can avail benefits in both Public and Private empanelled facilities.
- Under this Ayushman Bharat Scheme, govt. will make payment for treatment on “Package Rate Basis”.
- All the treatment cost will get included in Package Rates.
Ayushman Bharat Scheme is a Mega Health Insurance Scheme which will cover 10 crore families which includes around 50 crore people.
AB-NHPM Implementation
Cabinet Committee has made the following decisions to successfully implement the Ayushman Bharat Scheme.
- One of the core principles of AB-NHPM is Co-operative Federalism and Flexibility to states. There is a provision to partner the states through co-alliance.
- Under AB-NHPM, states will be free to choose the modalities for implementation. States can implement through Insurance Company or directly through Trust / Society or a Mixed Model.
- For giving policy directions and fostering coordination between Centre and States, cabinet committee proposed to setup Ayushman Bharat National Health Protection Mission Council (AB-NHPMC) at apex level chaired by Union Health and Family Welfare Minister.
- State would need to have State Health Agency (SHA) to implement the scheme.
- In partnership with NITI Aayog, a robust, modular, scalable and Inter-operable IT Platform will become operational which will entail a paperless and cashless transaction.
State / Districts Covered under AB-NHPM
AB-NHPM will get rolled out in all States / UTs in all districts with an objective to cover all targeted beneficiaries. NHPS Council will cooperate with various central government ministeries and State / UT governments who have already launched their own Health Protection Schemes for their own defined set of beneficiaries. There is a critical need to converge these schemes to achieve improved efficiency, reach and coverage.
PM Rashtriya Swasthya Suraksha Mission – Official Website
— For more details on the National Health Protection Scheme / Modicare / Ayushman Bharat Yojana / Pradhan Mantri Rashtriya Swasthya Suraksha Mission, visit the official website – www.pmjay.gov.in
National Health Protection Scheme (NHPS) – Rs. 5 Lakh per Family by Central Govt. (1 February 2018)
Central government in its union Budget 2018-19 has launched the much awaited National Health Protection Scheme (NHPS). Subsequently, govt. will provide Rs. 5 lakh to each family for secondary and tertiary hospitalization. Accordingly, this mega Health Protection Scheme / Ayushman Bharat Scheme announced in Union Budget 2018-19 will benefit around 10 crore families (50 crore people) across the country.
Ayushman Bharat Programme (NHPS) is the worlds biggest govt. funded health care scheme. Moreover in this Union Budget 2018, govt. has allocated Rs. 48,878 crore for the health-care sector which was 39,879 crore in the previous budget of FY 2017. Central govt. is going to start NHPS Scheme from 15 August 2018 or 2 October 2018. Moreover, the annual premium of Ayushman Bharat Scheme is around Rs. 900 to Rs. 1000 for each family as per the estimates of NITI Aayog.
First Health and Wellness Center is opened at Jangla, district Bijapur, Chhattisgarh. Treatment Package Rates for 1352 medical inspection and surgeries are finalized by the govt. and will soon be uploaded on the NHPM Portal. Central govt. will make NHPS Beneficiaries Selection on the basis of Socio-Economic and Caste Census Data – SECC 2011.
Central govt. is going to set-up 1.5 lakh health and wellness centers and community healthcare clinics under Bharat Ayushman Programme. For this programme, govt. will allocate Rs. 1200 crore and will also provide treatment for non-communicable diseases. Furthermore, govt. will also focus on including private enterprises to join the programme as a part of Corporate Social Responsibility (CSR) Initiatives.
PM National Health Insurance Scheme May Cost Over Rs 8000 Crore (Update on 27 August 2016)
The upcoming mega health insurance scheme termed as “Prime Minister National Health Insurance Scheme” may generate a premium of over Rs. 8000 Crore for the insurance companies. Under the new proposed scheme, the health ministry would require a financial support from 4000 to 5000 crores in order to pay the premium.
Under the current Rashtriya Swasthya Bima Yojana (RSBY), BPL families are covered for an insurance of up to Rs. 30,000 which will be phased out one the new scheme is launched. Under the RSBY scheme, there were about 1.18 crore hospitalizations till the end of last financial year.
Under the new PM National Health Insurance Scheme, the central government would pay 60% of the premium amount while the rest would be paid by the state governments. At present, under the RSBY, state governments pay only 25% of the premium amount while 75% is paid by the central government. Treatment Package Rates for 1352 medical inspection and surgeries are finalized by the govt. and will soon be uploaded on the NHIS Portal.
The guidelines for the operations and implementation of PM national health insurance scheme is being prepared by the health ministry. The ministry would soon start the process of empaneling the insurance companies and hospitals for the scheme. The mega health insurance scheme was announced by the PM on 15 August 2016 and will soon see the light of the day.
Announcement of National Health Insurance Cover for Poor (Update on 16 August 2016)
Narendra Modi, in his Independence day speech on 15 August 2016 announced that central govt. will start National health insurance scheme for poor. At that time, the scheme was named as “National Health Insurance Scheme” which aims to provide a health insurance cover of up to Rs. 1 Lakh to the poor.
The scheme was to benefit about 10 Crore families in the first phase. The main beneficiaries of the scheme were the families belonging to the BPL category or those in the list of deprivations as per socio-economic caste census data. Earlier named as NHPS, the scheme got a new name upon the launch.
Ayushman Bharat Health Scheme – PM Jan Arogya Yojana [Important Points]
PM Narendra Modi has launched Ayushman Bharat Health Scheme from Ranchi, Jharkhand on the birth anniversary of national poet “Ramdhari Singh Dinkar” (23 September 2018). Under this PM Jan Arogya Yojana (PMJAY), central govt. is going to provide cashless & paperless treatment of upto Rs. 5 lakh for secondary and tertiary hospitalization. National Health Protection Scheme (NHPS) will benefit 10 crore poor families and beneficiaries can avail treatment in all govt. / private empanelled hospitals.
Treatment of around 1300 diseases will be provided to beneficiaries at NHPM treatment package rates. AB-NHPM is a mega health insurance scheme to benefit 50 crore people whose name appears in Socio-Economic Caste Census (SECC) 2011 data. Ayushman Mitras will be trained and remain present at each hospital to assist people in getting claim settlement without any hassle.
It is imperative to note that there is no need to make any registration or fill online application form under PMJAY. People can avail treatment by just showing either their Aadhar Card or Ayushman Family Cards or Ration Card or Voter Card. In case of any problem contact the PMJAY helpline number at 14555 or 1800-111-565. This scheme is launched simultaneously in 445 districts of 30 states across the country.
Ayushman Bharat Health Scheme (AB-PMJAY) Launched by PM Modi
PMJAY-Ayushman Bharat is the biggest government sponsored healthcare scheme in the world. This scheme is not based on caste, gender or religion but includes deprived rural and urban families. In the upcoming days, this health assurance scheme will benefit lower middle class, middle class and upper middle class people by providing them indirect jobs. The central govt. believes that this “Modicare” scheme will become a game changer for the next general elections. The summary of extent and importance of the scheme are explained in brief below:-
1. Who will be the AB-PMJAY Beneficiaries
AB-PMJAY scheme targets at poor, deprived rural families and identified occupational categories of urban workers families. Accordingly if we go by the SECC 2011 data, this Ayushman Bharat Health scheme would include 8.03 crore households in rural areas and 2.33 crore families in urban areas.
The central govt. will ensure that no eligible beneficiary is left out (especially women, children and senior citizens). In addition to this, there is no cap on the family size and age of people under PM Rashtriya Swasthya Suraksha Mission (PMRSSM). People can check name in PMJAY beneficiaries list to check whether they are eligible or not.
2. How much will Ayushman Bharat Yojana Cost?
From current year, it is expected that it is costing around Rs. 10,000 crore. In a single year, there are likely to be around 8 crore beneficiaries and govt. targets to cover around 10 crore people in a single year by FY 2022.
Ayushman Bharat – PM Jan Arogya Yojana will run on a 60:40 basis where central govt’s share is around 60% and 40% share is of state government.
As per the reports of international rating agency Moody’s, Ayushman Bharat Yojana is credited positive for insurance companies as AB-NHPM scheme would result in higher premium growth. Moreover, NHPS scheme will also provide insurers with cross-selling and servicing opportunities.
3. Extreme outreach of Ayushman Bharat National Health Protection Scheme
All the states were asked to setup kiosks at all empanelled hospitals with PM-JAY branding. This initiative will cover all such hospitals with publicity material like banners on AB-PMJAY scheme, giving uniforms to Arogya Mitras who will help people about NHPS scheme at hospitals and distribute pamphlets to incoming patients.

The state govt. would also perform outdoor advertising and would hold panchayats in villages. This branding would assist beneficiaries to know where to contact to get PMJAY services. Publicity of AB-NHPM scheme, especially the audio and visual communication, will help in reaching the beneficiaries effectively.
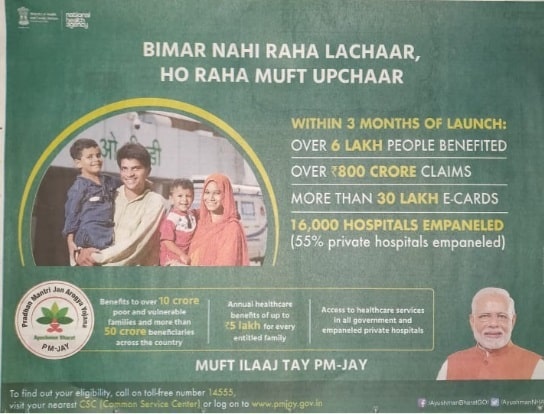
People who are still finding it difficult to understand the details of PMJAY scheme can contact the AB-PMJAY helpline number – 14555. Around 1.5 lakh Health & Wellness Centers will be opened across the country to provide appropriate treatment to the needy people.
Ayushman Bharat Yojana Review – Success or Failure (Analysis)
Ayushman Bharat Yojana or Pradhan Mantri Jan Arogya Yojana is a flagship scheme of the Modi government which was launched to provide proper healthcare to all the poor citizens. But here we are going to tell you the detailed analysis of the PMJAY scheme and whether this scheme is a success or failure.
As this is a much hyped mega health insurance scheme and gained lot of popularity since its announcement by PM Modi from Lal Qila, people must know its actual details and its operational procedure. Under this scheme, the central govt. provide cashless treatment upto Rs. 5 lakh to 50 crore people.
Even the difficulties faced by the people while getting cashless treatment at the empanelled hospitals are mentioned in this post. Here we are listing the advantages and disadvantages of Ayushman Bharat – PM Jan Arogya Yojana.
Ayushman Bharat Yojana Disadvantages
1. Number of Empanelled Hospitals is Less
The number of hospitals empanelled under Ayushman Bharat Yojana are lesser. PMJAY is an optional scheme for the hospitals i.e it gives the private hospitals a choice to become empanelled or not. So, a large number of private hospitals are staying out and are not opting for the scheme. This is because the package rates are fixed for the treatment procedure which hospitals believe are not sufficient. Therefore, a large number of people who wants treatment in these specific hospitals are not getting AB-PMJAY scheme benefits. In our opinion, the central govt. must make it compulsory for all the hospitals to get empanelled in these hospitals.
2. Non-Awareness about Operational Details of Ayushman Bharat Yojana
People does not have the basic knowledge about the operational guidelines of the scheme. Poor people are getting Ayushman Bharat e-Cards at home, but are unaware of what to do with these health insurance cards. At all the empanelled hospitals, Arogya Mitras are not present even during the daytime which is causing problems to a large number of people. So, there must be an authority which should keep a check on these Arogya Mitras whether they are discharging their duties with utmost sincerity or not.
3. Middlemen & Fraudulent Websites Asking for Money for PMJAY Scheme
Some people and websites are asking for money to include the name of non-beneficiaries in the Ayushman Bharat Scheme. It is imperative to note that Ayushman Bharat Yojana is an eligibility based scheme and its beneficiaries are already identified by the central government. The complete list of PMJAY beneficiaries is available at mera.pmjay.gov.in website under Am i eligible section. People must not fell prey to such unauthorized people and fraudulent websites which are asking for money as there is no application procedure for PMJAY enrollment.
4. Hospitals Doing Fraud in PM Jan Arogya Yojana
Some empanelled hospitals are creating patients on their own and are doing fraud. This is a reality as those people who are completely alright and their name appears in the SECC 2011 data are doing contracts with the hospitals. The contract is about the treatment that the hospitals will show that the person is ill and requires treatment and person is admitted in their hospitals. Then these hospitals make huge bills of treatment and gets it from the government and the person gets margin (10% or 20% of the total bill) from the hospitals. Thus this type of corruption in Ayushman Bharat Scheme is preventing its benefits to reach the needy people (intended beneficiaries).
5. OPD Fees Not Included in Ayushman Bharat – PMJAY Scheme
Another major disadvantage is that OPD fees for consulting doctors is not included under the Ayushman Bharat Yojana package. Moreover, people must remain admitted in the hospitals for at-least 2 days to claim scheme benefits which is a drawback. In case of minor diseases like fever which can be treated with medicines only are not included in this scheme.
Ayushman Bharat Scheme Benefits
The primary objective behind the launch of Modicare scheme was to provide cashless treatment upto Rs. 5 lakh to all poor families. So, the central govt. has fixed a minimum requirement that in case the name of the family appears in the SECC 2011 list, then all such people can avail free treatment at govt. / private hospitals. Around 10 crore families (over 50 crore people) are included in this scheme.
Scope / Coverage of PMJAY Beneficiaries
Modicare scheme has many benefits such as it includes all the pre-existing diseases. The coverage of PMJAY scheme also includes diagnosis, operation, treatment fees along with pre-hospitalization and post hospitalization charges in some cases. The list of those things which are outside the scope of treatment is very small.
Final Opinion of Ayushman Bharat Yojana
So in our opinion, this health insurance scheme is launched with good intention and to provide treatment to every poor people. But some people are trying to rule out its advantages and make it a failure. The central government has issued complete guidelines about every aspect of this scheme but has not reached to all the people. Accordingly, there is a need to create mass awareness about the Pradhan Mantri Jan Arogya Yojana and to let people know that how could they get benefits of this scheme.
In the near future, if the scheme is implemented correctly without corruption practices then it would be a completely successful and worlds largest healthcare scheme. But in case the scheme is not implemented properly, then it would be a failure and would become like one of the many other previous government healthcare schemes.
from सरकारी योजना
via

0 टिप्पणियाँ